Chest:预测肺癌的慢性阻塞性肺疾病临床特征!
2018-02-14 xing.T MedSci原创
由此可见,COPD严重程度,包括气流阻塞、肺气肿和呼吸功能恶化都是肺癌的独立预测因素。这些危险因素应作为肺癌筛查生存获益的纳入标准和排除标准开展进一步研究。同时,需要进行研究来确定减少吸烟者呼吸功能恶化是否能降低肺癌风险。
肺癌是导致慢性阻塞性肺病(COPD)患者死亡和住院的主要原因,需要详细了解COPD的临床特征。近日,呼吸领域权威杂志chest上发表了一篇研究文章。该研究旨在确定有无COPD的吸烟者临床及影像学特点,这些特征是否与肺癌的发病风险增加有关。
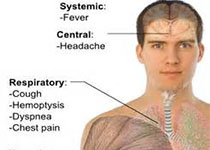
研究人员对携带和未携带肺癌基因的COPD患者进行了一项巢式病例对照研究,这些患者年龄为45-80岁,至少抽烟10包每年。基线评估包括:肺活量、高分辨率胸部CT和呼吸问卷。八年的纵向随访确定新发的肺癌诊断。肺癌患者以1:4的比例匹配年龄、种族、性别、吸烟史相似的对照者。多因素logistic回归分析用于确定预测肺癌的临床特征。
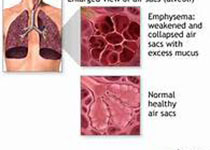
与未来肺癌风险相关的临床特征包括:降低的FEV1/FVC(每减少10%的比值比(OR)为1.28,95%可信区间(CI)为1.12-1.46)、肺气肿的严重程度(OR为2.31,95%CI为1.41-3.86)、进入研究前的呼吸加重(每增加一次事件的OR为1.39,95%CI为1.04-1.85)。呼吸加重也与小细胞肺癌组织学类型相关(OR为3.57,95%CI为1.47-10)。
由此可见,COPD严重程度,包括气流阻塞、肺气肿和呼吸功能恶化都是肺癌的独立预测因素。这些危险因素应作为肺癌筛查生存获益的纳入标准和排除标准开展进一步研究。同时,需要进行研究来确定减少吸烟者呼吸功能恶化是否能降低肺癌风险。
原始出处:
Laurie L. Carr,et al. Features of Chronic Obstructive Pulmonary Disease as Predictors of Lung Cancer.chest.2018. https://doi.org/10.1016/j.chest.2018.01.049
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床特征#
25
#EST#
32
#阻塞#
25
#Chest#
57