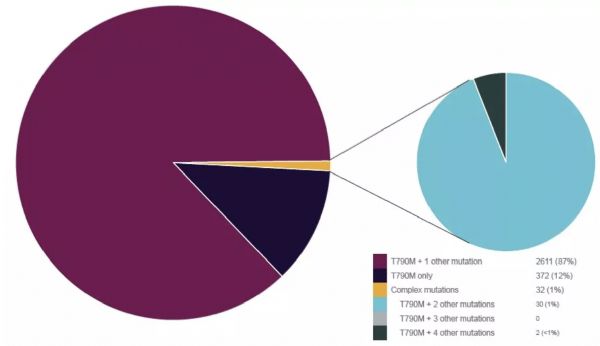
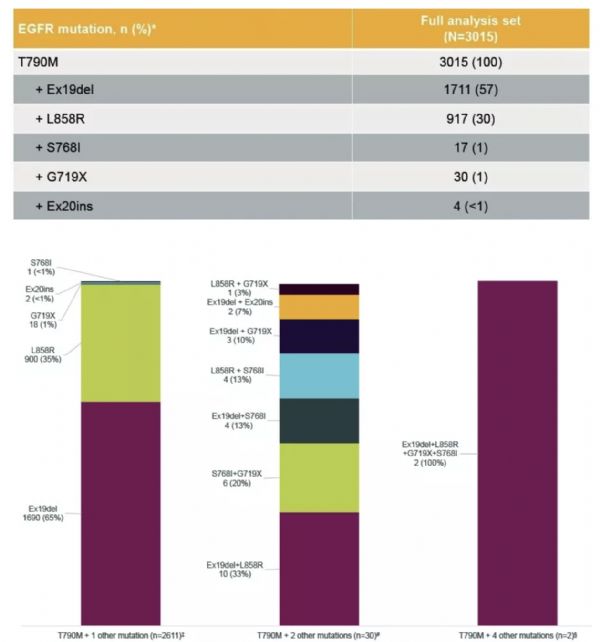
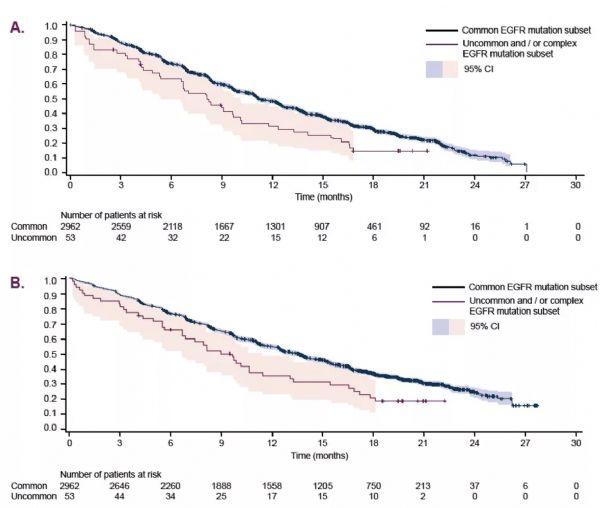
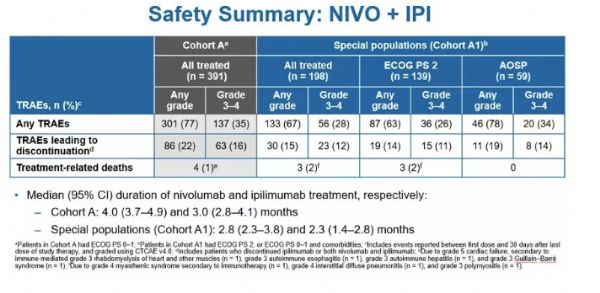
2019 WCLC ∣ 奥希替尼治疗T790M阳性伴罕见和/或复杂突变的晚期NSCLC,疗效显著
2019-09-15 肿瘤资讯 良医汇-肿瘤医生APP
2019年9月7~10日,由国际肺癌研究协会(IASLC)举办的2019年第20届世界肺癌大会(WCLC)在西班牙巴塞罗那盛大召开。当地时间9月8日上午,在壁报展示专场(Poster Session)上,来自加拿大多伦多大学的Parneet K. Cheema教授展示了“奥希替尼用于T790M阳性晚期非小细胞肺癌(NSCLC)的真实世界研究:来自罕见/复杂突变亚组患者的分析(ASTRIS研究)”的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#T790M#
35
#WCLC#
40
#晚期NSCLC#
43
#罕见#
33
谢谢梅斯提供这么好的信息,学到很多
51
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
51