JACC:接受TAVR术的晚期肾脏疾病患者预后研究
2019-06-21 不详 MedSci原创
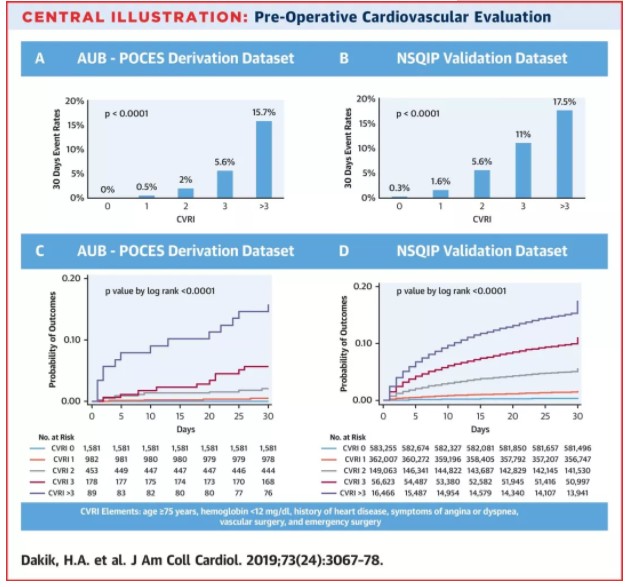
对于晚期肾脏疾病(ESRD)患者,外科主动脉瓣置换术会增加患者的死亡和不良事件风险,本研究的目的旨在评估经皮经导管主动脉瓣置换术(TAVR)在ESED患者中的预后。在美国心脏病学会数据库中的72631名接受TAVR治疗的严重主动脉瓣狭窄(AS)患者中,3053名(4.2%)患者患有ESRD。与非透析患者相比,ESRD患者更年轻(76岁vs 83岁; p < 0.01),预测的死亡风险更高(1
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AVR#
30
#晚期肾脏疾病#
33
#疾病患者#
30
#JACC#
27
#患者预后#
39
#ACC#
38