心血管疾病等危症——糖尿病如何管理?控制胆固醇居首位
2018-08-02 国际循环编辑部 国际循环
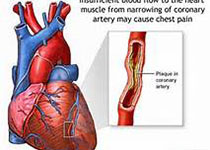
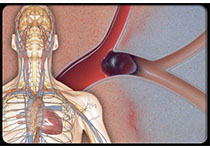
编者按:糖尿病是心血管疾病(CVD)的等危症,二者关系极为密切。对于糖尿病的管理,中华医学会糖尿病学分会副主任委员、上海长海医院邹大进教授曾结合2017版《中国2型糖尿病防治指南》提出了新“五驾马车”理论,即控制胆固醇、控制血压、血糖管理、体重管理、抗血小板治疗。邹教授同时指出,对于糖化血红蛋白(HbA1c,A)、血压(Blood Pressure,B)和胆固醇(Cholesterol,C)的重视
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血管疾病#
20
好好好好好好好好
46
学习了,谢谢分享。
51
谢谢分享,一点一点的学习,一点一点的积累,一点一点的进步
49
谢谢MedSci提供最新的资讯
43
学习了很有用
45
学习了
41