Cancer Cell:多梳抑制复合体1能够驱使双阴性前列腺癌的转移
2019-09-07 AlexYang MedSci原创
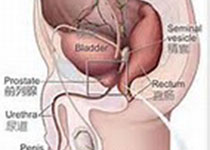
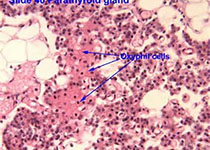
最近,有研究人员阐释了多梳抑制复合体1通过协调干细胞和免疫抑制,能够驱使双阴性前列腺癌转移的机制。目前,转移位点的免疫逃避机制仍旧不清楚。他们展示了多梳抑制复合体1(PRC1)能够促使双阴性前列腺癌(DNPC)中骨骼和内脏器官的定植。体内遗传筛选鉴定了CCL2是PRC1诱导的首要促转移基因。CCL2能够调控自我更新和诱导类M2肿瘤相关巨噬细胞和调节性T细胞的招募,从而通过免疫抑制和血管生长来协调转
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
21
#Cell#
31
#复合体#
28
#cancer cell#
33
前列腺癌相关研究,学习了,谢谢梅斯
43