Lancet:双侧颈内动脉血栓形成是怎么回事?
2018-07-07 杨中华 脑血管病及重症文献导读
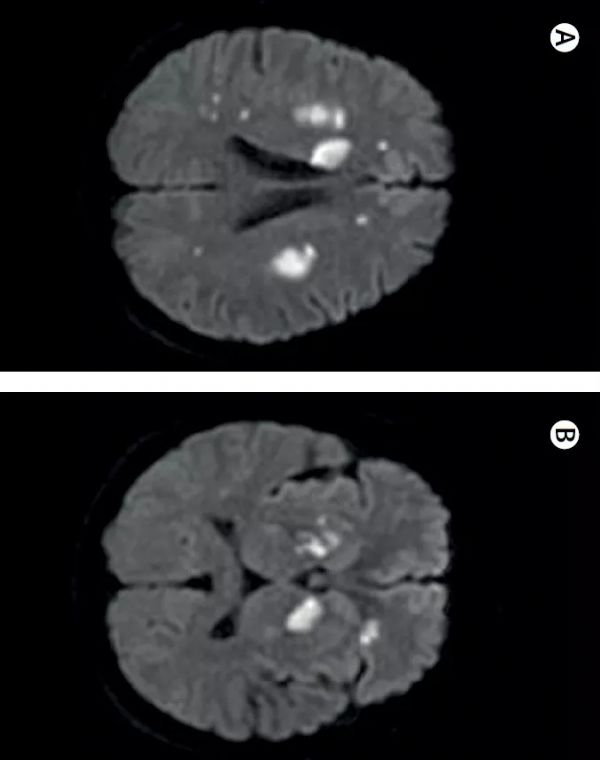
51岁,男性。 因认知能力下降两天到急诊室就诊。 首次脑CT未见异常,但是2天后MRI显示双侧额叶、半卵圆中心、脑室周围、基底节梗死(下图A和B)。
51岁,男性。
因认知能力下降两天到急诊室就诊。
首次脑CT未见异常,但是2天后MRI显示双侧额叶、半卵圆中心、脑室周围、基底节梗死(下图A和B)。
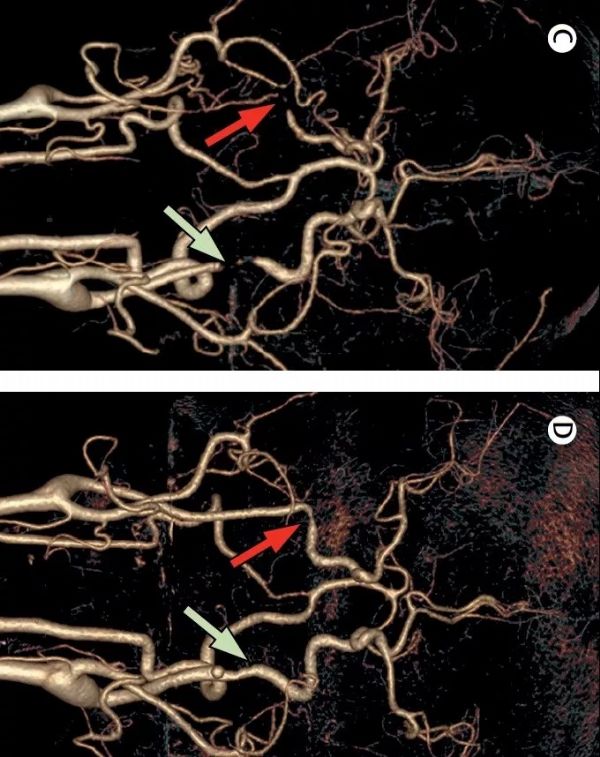
头颈CTA显示右侧ICA完全闭塞(下图C),左侧ICA严重狭窄残留10%管腔通畅。
血细胞计数和代谢方面检查正常。
易栓症检查发现抗心磷脂抗体IgM升高:首次为55 U/ml,3个月后为51 U/ml(正常值小于12 U/ml)。抗心磷脂抗体IgG首次为3.5 U/ml;3个月后为4 U/ml(正常值小于12 U/ml)。狼疮抗凝物实验阴性,抗-β2糖蛋白I IgG抗体皆正常。
诊断为抗心磷脂抗体综合症,开始低分子肝素抗凝治疗,后改为Vit K拮抗剂(目标INR 3-4)治疗。3周后,患者的认知功能包括定向力、语言、计算和记忆力皆显著改善。复查头颈CTA显示双侧ICA部分再通(上图D)。
原始出处:
Fei Xiao, Xin Tian, Xue-feng Wang. Antiphospholipid syndrome causing reversible internal. Lancet 2018; 391: 2641
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉血#
28
#Lancet#
28
#双侧#
30
#动脉血栓#
27
#动脉血栓形成#
20
#动脉血栓形成#
32
#颈内动脉#
32
学习了
53
好文献学习了
54