PLOS ONE:肿瘤微环境如何促进乳腺癌细胞迁移
2018-04-01 海北 MedSci原创
肿瘤微环境(TME)可以促进肿瘤细胞的侵袭和转移。促癌微环境转化的一个重要步骤是正常基质成纤维细胞向癌相关成纤维细胞(CAF)的转化。
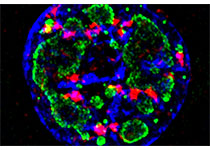
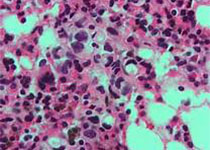
肿瘤微环境(TME)可以促进肿瘤细胞的侵袭和转移。促癌微环境转化的一个重要步骤是正常基质成纤维细胞向癌相关成纤维细胞(CAF)的转化。CAF存在于大多数实体瘤中,并且可以分泌细胞因子,趋化因子和生长因子到TME中,直接促进肿瘤细胞的转移。 但至今为止,TME对移动性肿瘤细胞中细胞骨架调节的确切作用仍然是个谜。
保守的formin细胞骨架调节蛋白家族在非分支肌动蛋白丝的装配和/或捆绑中起着重要的作用。哺乳动物的mDia2 / DIAPH3 / Drf3 / Dia可以组装成为一个动态的F-肌动蛋白细胞骨架,它是肿瘤细胞迁移和侵袭的基础。
因此,来自托莱多大学健康科学院的研究人员试图了解CAF衍生的趋化因子是否通过修饰由formin组装的F-肌动蛋白细胞骨架,进而影响乳腺肿瘤细胞的运动性。
在MDA-MB-231细胞中,相对于正常人类乳房成纤维细胞(HMF)的条件培养基(CM),来自WS19T CAF(人乳房肿瘤相邻CAF系)的条件培养基能够显着并强烈增加伤口闭合和细胞侵袭性。与对照HMF-CM和WS21T CAF-CM(该乳腺CAF细胞系未能促进稳健的MDA-MB-231迁移)相比,WS19T-CM还促进了MDA-MB-231细胞中蛋白酶体介导的mDia2降解。
相对于对照WS21T CM,细胞因子阵列分析鉴定了WS19T CM中上调的分泌因子。研究人员将CXCL12鉴定为影响mDia2蛋白丢失的CM因子,这增加了MDA-MB-231细胞的迁移。
这些数据表明,CAF通过CXCL12的分泌,以调节乳腺肿瘤细胞中mDia2-定向的细胞骨架的机制,促进肿瘤细胞的迁移和侵袭。
原始出处:
Kaitlyn M. Dvorak et al. Carcinoma associated fibroblasts (CAFs) promote breast cancer motility by suppressing mammalian Diaphanous-related formin-2 (mDia2). PLOS ONE, 2018; DOI: 10.1371/journal.pone.0195278
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Plos one#
37
#迁移#
44
#癌细胞#
43
#细胞迁移#
49