JAMA Oncol:乳腺癌放疗敏感性预测“利器”--循环肿瘤细胞CTC!
2018-05-07 肿瘤资讯编辑部 肿瘤资讯
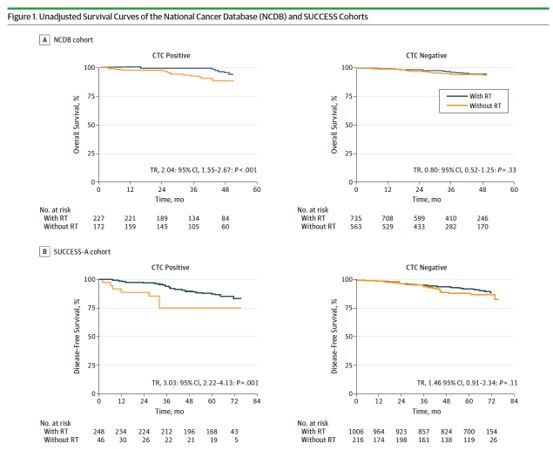
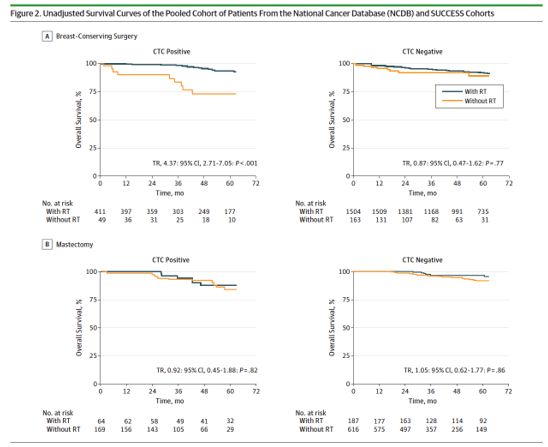
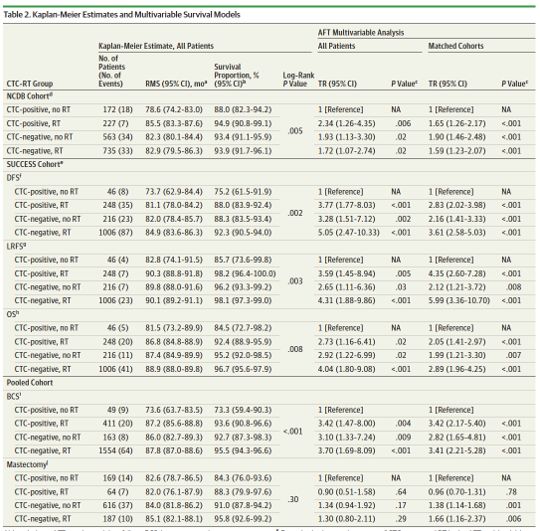
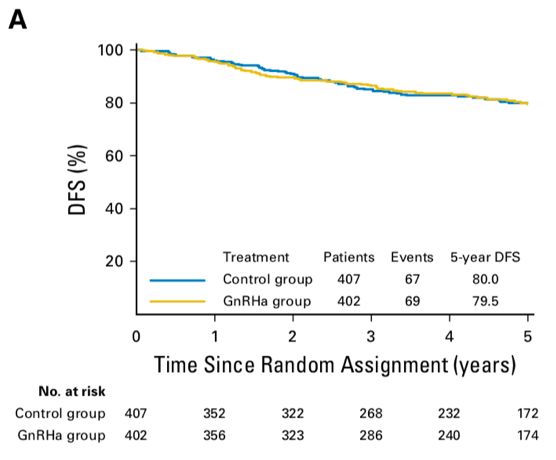
目前,尚无有效的生物标志物可以预测早期乳腺癌患者接受放疗的获益。CTC状态是乳腺癌的重要预后标志物。近期一项发布在《JAMA Oncology》的研究探索了CTC状态能否早期乳腺癌的放疗获益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
37
#CTC#
33
#肿瘤细胞#
32
#敏感性#
22
#循环肿瘤细胞#
31
阅
77
学习学习谢谢分享
65
学习了很有用
71
了解了解.学习学习
86
学习了
70