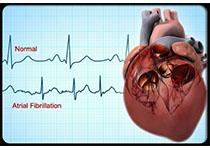
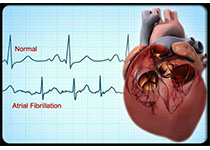
JAHA:心肌离子通道病患者可放心接受牙科治疗
2019-07-26 国际循环编辑部 国际循环
约1/3不明原因心脏猝死由Brugada综合征和长-QT间期综合征所致。由于使用利多卡因带来的潜在生命危险,心肌离子通道疾病患者通常对牙科治疗存在顾虑。近期发表于《美国心脏协会杂志》(Journal of the American Heart Association)的研究提示,利多卡因联合或不联合肾上腺素进行局部牙科麻醉是安全的,不会导致通道病变患者出现危及生命的心律失常。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#牙科治疗#
26
#离子通道病#
35
#AHA#
28
#牙科#
29
#离子通道#
45
mark
74