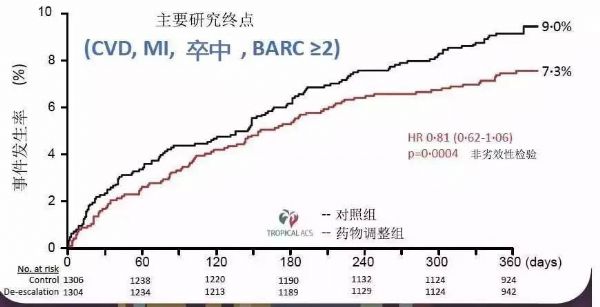
Lancet:ACS患者PCI术后,由普拉格雷调整为氯吡格雷维持应用12个月临床获益更佳
2017-08-28 阿拉蕾 中国医学论坛报
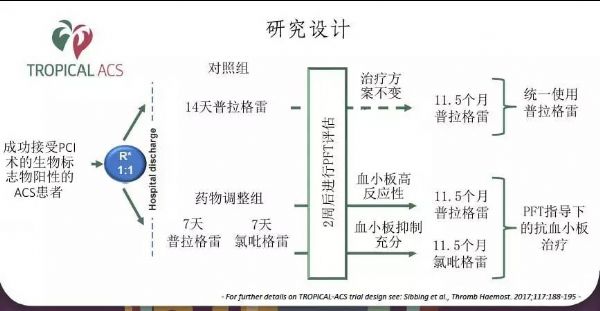
ESC大会第二天,西班牙时间8月27日14点30分,北京时间8月27日20点30分,备受瞩目的TROPICAL-ACS研究结果发布,同时在线发表于柳叶刀杂志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Lancet#
20
#PCI术#
27
#临床获益#
33
#ACS#
26
#PCI术后#
28
#ACS患者#
28
学习了谢谢分享
66
学习了.谢谢
0
学习了谢谢分享
61
为什么是非劣效研究?
59