2018欧洲高血压指南发布!郭艺芳教授的点评如此精彩!
2018-06-11 佚名 医师报
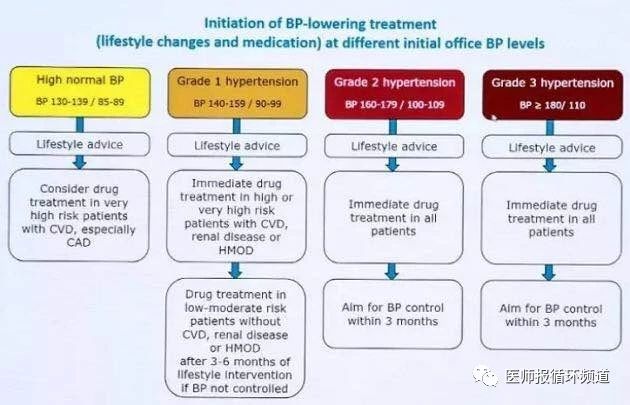
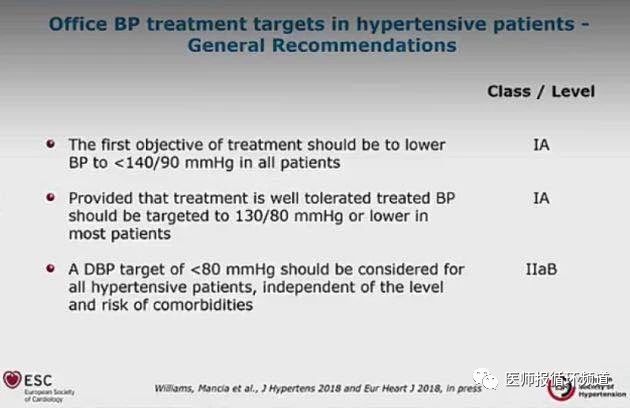
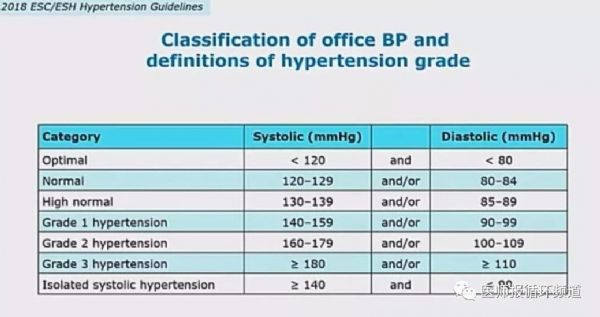
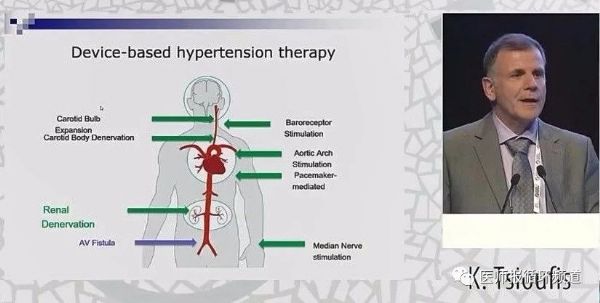
西班牙当地时间6月9日,2018 欧洲高血压学会(ESH)年会召开,会上发布了由ESH和欧洲心脏病学会(ESC)共同制定的ESC-ESH 2018高血压指南。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













好
67
好
66
好
70
学习指南.依据:指南.
63
#高血压指南#
45
#欧洲#
24
谢谢了.学习
66
好
29
谢谢分享!
32
谢谢分享.学习了
33