慢性自发性腰椎管内硬膜外血肿1例
2018-02-14 王拴池 中国骨伤
作者:沧州中西医结合医院脊柱脊髓外科 王拴池临床资料 患者,男,77岁,因“腰痛伴双下肢麻木、疼痛、无力8年,加重2个月”于2016年11月7日入院。患者8年前腰痛,伴双下肢麻木、无力,间歇性跛行,2个月前无明显诱因出现腰痛明显加重伴双侧臀部疼痛,站立行走时疼痛明显,并伴尿频、尿急。查体:腰背部压痛、叩痛明显,伴双侧臀部放射痛,腰椎屈伸活动受限明显,右小腿及足部针刺觉减弱
作者:沧州中西医结合医院脊柱脊髓外科 王拴池
临床资料
患者,男,77岁,因“腰痛伴双下肢麻木、疼痛、无力8年,加重2个月”于2016年11月7日入院。患者8年前腰痛,伴双下肢麻木、无力,间歇性跛行,2个月前无明显诱因出现腰痛明显加重伴双侧臀部疼痛,站立行走时疼痛明显,并伴尿频、尿急。查体:腰背部压痛、叩痛明显,伴双侧臀部放射痛,腰椎屈伸活动受限明显,右小腿及足部针刺觉减弱,双侧胫前肌肌力Ⅳ级,双拇趾背伸肌力Ⅲ级,双足跖屈肌力Ⅲ级;双膝腱、跟腱反射未引出,双下肢直腿抬高试验阴性。
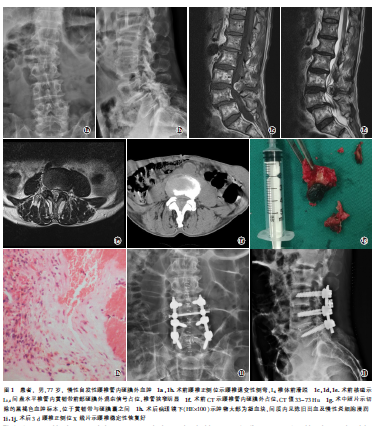
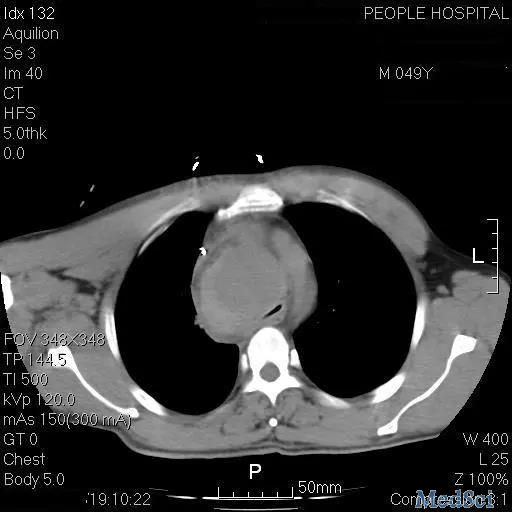
腰椎JOA评分7分。辅助检查X线:腰椎退变,L4椎体前滑脱(图1a,1b);腰椎CT及核磁:L3,4间盘水平椎管内黄韧带前部硬膜外混杂T1混杂T2信号,相应层面椎管面积变窄(图1c,1d,1e,1f);腰丛神经核磁平扫未见明显异常。双下肢肌电图未见明显异常。脑脊液常规、生化及免疫学检查均未见异常。男性肿瘤标记物未见异常。完善检查后考虑腰椎管狭窄、腰椎滑脱,且不排除黄韧带囊肿出血或椎管内血肿可能,于入院后第7天全麻下行腰椎后路椎板切除椎管探查+植骨融合内固定术。
手术方法:
插管全麻后取腰部后正中入路,显露L3-L5椎板、棘突,探查见L4椎体前滑脱,椎间不稳,遂于L3-L5椎体双侧置入椎弓根螺钉。去除L3下部、L4及L5上部椎板,见L3,4间盘水平部分黄韧带为暗黄褐色,切除椎板,见黄韧带与硬膜囊间黑褐色团块状质脆韧组织(图1i),大小约为1.2CM×1.0CM×0.8CM,与黄韧带腹侧及硬膜囊背侧粘连,小心剥离切除黄韧带及血肿块组织,硬膜囊背侧可见压痕及少量慢性肉芽增生组织,探查过程中未发现血肿来源,但其与椎管内静脉丛相邻。取出肿物组织送病理。再次探查肿物切除完整无残留,考虑L4-L5椎间滑脱不稳,行椎间融合,彻底冲洗及止血后,见硬膜搏动良好,减压充分。钛棒固定椎弓根螺钉,留置引流管。台下切开肿物,见肿物内部为黑褐色凝血块,部分已机化,术后给予激素、脱水、营养神经药物等治疗。术后第1天腰痛及臀部疼痛症状较术前明显恢复,JOA评分20分。术后第7天腰痛及下肢疼痛症状消失。术后2周如期拆线、出院。术后病理(图1j):肿物大部为凝血块,间质内见陈旧出血及慢性炎细胞浸润。
讨论
自发性椎管内硬膜外血肿(SSEH)是指血液在硬脊膜外腔非特异性的聚集。并伴快速发展的脊髓、神经压迫症状,严重者甚至可在短时间内出现截瘫。该病临床上少见,占硬膜外占位性病变比例<1%,常为急性发病,可造成严重神经功能损伤。慢性者血肿者少见,临床上诊断困难,易出现漏诊及误诊。SSEH可发生在任何年龄阶段,以成人多见。发生的位置以颈、胸段最为多见,本例血肿出现在腰椎,较少见。有学者统计显示约33%患者出血原因不明,在有明确病因的病例中,长期抗凝药物及血管发育畸形为主要病因。本例患者无明确病因:无外伤史,无口服抗凝药物病史,未发现明确血管畸形证据。术中探查未发现血肿来源,但其与椎管内静脉丛相邻,考虑静脉丛来源可能性大。
SSEH的典型临床表现为病变节段位置的突发性颈胸腰背部疼痛,并可伴肢体放射痛,并出现病变节段支配区域以下运动、感觉障碍甚至二便障碍,严重者可发展为截瘫。而慢性椎管内硬膜外血肿多具有血肿体积小、压迫轻、椎管内容物容让性好等特点,就本病例而言,患者发病缓慢,临床症状、体征轻,且并无短时间内快速加重,与血肿体积小、腰椎管容积较大、马尾神经容让空间较大、马尾神经耐压迫能力较强等有关。
由于慢性椎管内血肿病例症状与脊柱退变性疾病如间盘突出症、椎管狭窄等症状类似,容易将其漏诊、误诊,而对于体积较小且发生时间较长的血肿,影像学检查有时难以区分,尤其是患者同时合并退变性疾病时。必须详细询问患者病史,包括外伤史、口服药物史、血液系统疾病史,排除凝血功能异常。辅助检查中核磁是最有意义且最快速有效的,因为核磁可清晰显示血肿位置及神经受压、损伤情况。相比MRI,CT存在一定不足:不能显示脊髓、神经受损情况,不能完全分辨硬膜与血肿关系。
MRI典型表现为:矢状位血肿呈带状或梭形,横断位则呈半弧形,血肿在急性期显示T1WI等信号,T2WI低信号;慢性期(>14d)中早期T1WI、T2WI为高信号,慢性晚期可出现呈低信号的含铁血红素沉积环,其为特征性表现。血肿多位于椎管侧后方、后方,其原因为硬膜腹侧空间小,静脉丛受压,不易出血,而硬膜背侧静脉丛丰富且压力较低,易发生出血形成血肿。本例血肿为类圆形团块,在T1WI为稍高信号,T2WI为高信号,提示血肿处于慢性期。而术后病理检查仍是SSEH最终确诊手段。
早期行椎板减压、血肿清除手术治疗是大多数学者的共识,多数病例术后恢复良好。国内部分学者认为对于血肿量小的患者保守治疗效果良好,但需严密观察患者神经功能情况,一旦病情加重应尽早手术干预。本病例患者血肿为与腰椎管内、且血肿体积较小,临床症状较轻,在2个月的血肿病史中症状无明显缓解,手术解除神经压迫后腰部疼痛及臀部放射痛症状迅速缓解,提示对于腰椎管内硬膜外血肿患者,慢性患者或急性患者保守治疗后症状缓解不理想者手术治疗效果仍有较好效果。
来源:中国骨伤2018年1月第31卷第1期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#椎管内#
28
#椎管#
23
学习了.谢谢作者分享!
66
#腰椎管内#
34
#硬膜外#
34
#硬膜外血肿#
34
学习了.引以为鉴.
57
受益匪浅.谢谢分享!
60
#腰椎#
25
#血肿#
28