Am J Infect Control:合理使用抗菌药物将降低万古霉素使用患者的死亡率
2018-01-10 检索:乔浦,翻译:宁梦,审核:孔懿 SIFIC感染官微
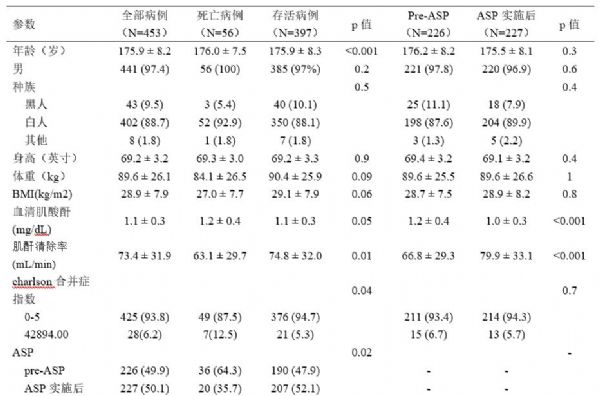
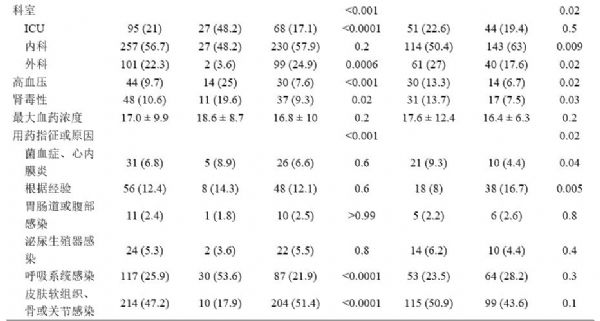
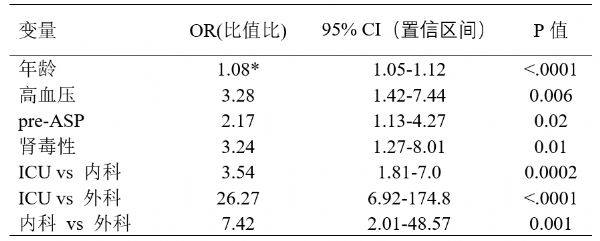
越来越多的研究证明,合理使用抗菌药物(通常被称为抗菌药物导向计划,Antimicrobial Stewardship Programs,ASP)能优化临床结局,减少使用抗生素带来的副作用,如可减少耐药菌感染,缩短住院时间,减少院内感染。现有大多数研究主要关注ASP实施后的费用降低、经济效益、减少不良反应,观察指标多是耐药率或感染率,较少有研究使用死亡率作为观察指标,特别是万古霉素服用后患者死亡率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#合理使用#
31
谢谢了.学习
66
学习谢谢分享!
44
#抗菌#
23
#抗菌药#
29
非常支持
55
好
51
学习了.涨知识
75
好好好好好好好好
30