腰椎管内哑铃型血管外皮瘤1例
2018-10-29 孙硕 张金凤 周辉 临床神经外科杂志
血管外皮瘤(hemangiopericytoma,HPC)是一种起源于血管和毛细血管周细胞的血管瘤,通常发生于皮下软组织和骨骼系统,而在中枢神经系统中很少发生,在椎管内更是罕见。仅仅占中枢神经系统肿瘤的1%。目前关于椎管内血管外皮瘤的报道仍较少。现报告1例腰段椎管内哑铃型血管外皮瘤患者,并结合国内外文献复习探讨其临床特点。
血管外皮瘤(hemangiopericytoma,HPC)是一种起源于血管和毛细血管周细胞的血管瘤,通常发生于皮下软组织和骨骼系统,而在中枢神经系统中很少发生,在椎管内更是罕见。仅仅占中枢神经系统肿瘤的1%。目前关于椎管内血管外皮瘤的报道仍较少。现报告1例腰段椎管内哑铃型血管外皮瘤患者,并结合国内外文献复习探讨其临床特点。
1.资料与方法
1.1一般资料
患者男性,46岁。因“左下肢疼痛3年,加重伴左下肢无力1个月”于2016年9月收治入院。患者3年前始无明显诱因出现左下肢疼痛不适,按腰椎间盘突出症治疗,服药未见效;约1个月前患者左下肢疼痛加重,并出现左下肢无力,双下肢痛觉减退,以左下肢明显。入院查体:左下肢肌力Ⅳ级,其他肢体肌力Ⅴ级;双下肢痛觉减退,以左下肢明显;四肢肌张力正常,双侧病理征阴性。术前腰椎MRI平扫+增强示:L1-2椎管内占位,肿瘤从椎间孔突出,呈哑铃型,T1WI和T2WI呈等信号;增强后见肿瘤均匀强化(图1)。

图1 术前腰椎MRI检查。A、B:矢状位;C:冠状位;D:轴位
1.2手术方法
手术采用后正中入路,患者取右侧俯卧位,左侧在上。按照术前X线定位好腰1-2椎体水平后,取腰后正中切口约12 cm;依次分离皮肤、皮下组织及肌肉后,充分暴露棘突及椎板,用铣刀铣下第1、2腰椎棘突及椎板后,见肉红色肿瘤位于硬脊膜外左侧,血供丰富;分离肿瘤与硬脊膜边界,将硬脊膜外肿瘤全切除(图2)。
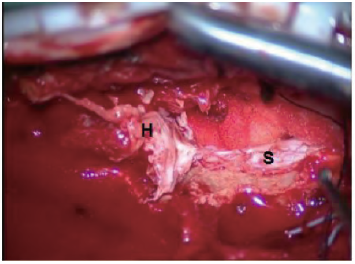
图2 肿瘤切除术中所见;注:H-血管外皮瘤,S-脊髓
由于从椎间孔突出至腹膜后的肿瘤较大,考虑到一次性完整切除的手术难度大,以及患者耐受能力差,故暂予椎管内肿瘤全切除,待患者恢复后转至泌尿外科行二期手术治疗。
2.结果
术后患者的左下肢疼痛消失,左下肢肌力与术前相仿,双下肢痛觉减退较术前好转。术后1个月复查腰椎MRI示,椎管内肿瘤切除完整,未见复发(图3)。
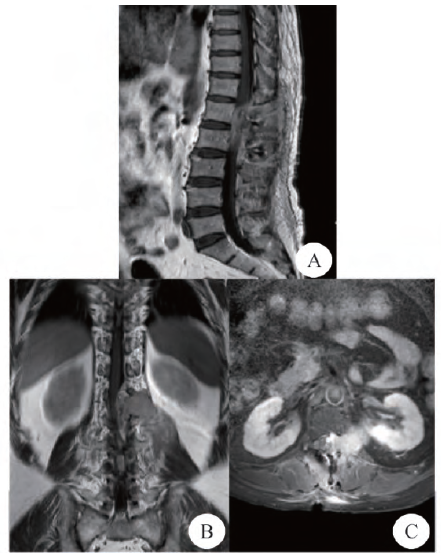
图3 术后1个月MRI复查,椎管内肿瘤全部切除。A:矢状位;B:冠状位;C:轴位
术后半年随访,患者四肢肌力恢复至Ⅴ级,双下肢痛觉恢复正常。术后病理检查显示,肿瘤组织以血管为中心血管外皮细胞增生,核呈异性分裂,有丝分裂相明显,瘤细胞被大量的窦状血管围绕;免疫组化示,肿瘤细胞CD34(3+)、CD99(3+)、VIM(3+)、BCL-2(3+)、SMA(1+)、CD31(-)、S-100(-)、Desmin(-)、KI-67约15%+;诊断为:血管外皮瘤(图4)。
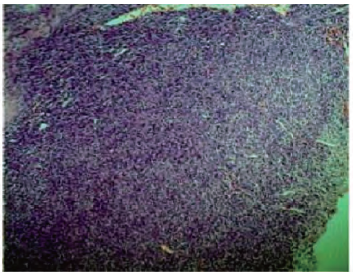
图4 术后病理学检查
3.讨论
血管外皮瘤是一种少见的具有侵袭性的肿瘤,被认为是起源于毛细血管和小静脉内皮细胞周围齐默尔曼周细胞的一种间质性肿瘤。随着对其研究的深入,逐渐发现其与孤立性纤维性肿瘤的组织学特征相似,甚至可以看作是同一种肿瘤。因此,在最近的WHO肿瘤分类系统中,血管外皮瘤被列为孤立性纤维性肿瘤的一种变异体。其可发生于身体任何部分,但最常见的部位是四肢、骨盆、腹腔及头颈部,很少在中枢神经系统中出现。自Stout和Murray在1942年首先发现后,只有大约80例椎管内血管外皮瘤病例被报道。
本研究回顾1例椎管内血管外皮瘤患者的临床资料,并复习国内外文献,探讨腰椎管内血管外皮瘤的临床、影像学和病理学表现,以及治疗方法、预后和分型等方面的特点。
3.1发病及临床特点
椎管内血管外皮瘤因比较罕见,缺乏大量的临床病例及相关研究报道,其发病特点并不是很明确。但从目前的文献报道中总结显示,椎管内血管外皮瘤可发生于任何年龄,多发生于青壮年,平均发病年龄在34岁左右,男性多于女性。肿瘤发生部位主要在颈椎及胸椎,腰椎、骶椎则较少发生,但差异并不是非常明显;发生在椎管内的血管外皮瘤多累及2~3个节段。
其临床特点:(1)起病表现及病程无明显特异性,多见四肢疼痛症状;(2)相关脊髓节段的神经根刺激症状或脊髓受压症状突出,常为首发症状;(3)临床表现主要取决于肿瘤的大小及肿瘤的位置,而与组织病理分型无关。本例患者为中年男性,以下肢疼痛为首发症状;MRI检查显示肿瘤位于椎管内,且分布在腰1-2椎体节段,符合椎管内血管外皮瘤的发病情况及临床特点。
3.2分型及影像学表现
椎管内血管外皮细胞瘤共分为3大类和5个亚型。Ⅰ型是硬膜外血管外皮细胞瘤(ⅠA位于椎管内,ⅠB位于椎管外),Ⅱ型是硬膜内血管外皮细胞瘤(ⅡA位于髓外,ⅡB位于髓内),Ⅲ型是硬膜内血管外皮细胞瘤扩展到硬膜外及椎旁区。大多数椎管内血管外皮瘤的影像学表现是非特异性的,具有与其他颅内或椎管内肿瘤相似的影像学特征。CT检查通常显示为硬膜病变,无特殊的表现。MRIT1WI及T2WI上均表现为等信号,增强扫描病变呈均匀强化。血管外皮瘤与其他肿瘤鉴别十分困难。
Ⅰ型和ⅡA型血管外皮瘤需要与脑膜瘤及神经鞘瘤相鉴别;与脑膜瘤相比,血管外皮瘤没有钙化,表现骨性增生及基底狭窄的椭圆形状。神经鞘瘤在MRIT2WI上可见到流体信号增强,在MRIT1WI增强上呈现边缘强化,而血管外皮瘤在MRI上则表现为等信号及均匀增强信号。ⅡB型血管外皮瘤需要与室管膜细胞瘤及血管母细胞瘤相鉴别;一些ⅠB型和Ⅲ型血管外皮瘤可侵及椎体及椎板等结构,可协助诊断。除了需要与这些主要的疾病鉴别外,还有与淋巴瘤、转移瘤、肉瘤、孤立的神经纤维瘤及胶质瘤的相鉴别也应考虑。
3.3病理学表现
椎管内血管外皮瘤没有特殊的影像学及临床表现,其诊断非常困难。因此,需综合临床、影像学表现及病理检查做出诊断,组织病理学检查至关重要。病理学检查常表现为以血管为中心血管外皮细胞增生,核呈圆形、椭圆形或梭形分裂相,有丝分裂相明显,瘤细胞被大量的窦状血管围绕,可见典型的鹿角状的管腔。免疫组化检查被认为是区分与其他肿瘤的一种有效的方法。免疫组化检查示,肿瘤CD34、CD99、Bcl-2、HLA-DR、Leu-7、波形蛋白及ⅩⅢa因子均可表达阳性,S-100蛋白、CK、EMA、PR、CEA和Desmin表达阴性,但偶尔也可见S-100蛋白、Desmin、CK表达阳性。
本例患者术后病理学检查显示,以血管为中心血管外皮细胞增生,核呈异性分裂,瘤细胞被大量的窦状血管围绕等特征;免疫组化检查示CD34、CD99及Bcl-2等阳性表达;符合血管外皮瘤的病理特征。
3.4治疗及预后
外科手术治疗被认为是中枢神经系统血管外皮瘤的首选治疗方法,目前认为比较有效且应作为治疗目标的手术方式是全切除。具有清晰的边缘和膜的肿瘤更应将其完整切除。有文献指出,肿瘤全切除者的5年生存率明显高于部分切除者,DFS明显延长;但ⅠB和Ⅲ型高级别肿瘤由于其常侵及椎体、椎板甚至棘突,因此全切除率较低;另外高危患者则不建议手术治疗。
血管外皮瘤的血供非常丰富,术中出血量大,给手术者带来很大的挑战,这可导致手术后的高复发率、死亡率,以及肿瘤切除不完整的高风险。因此,有些人建议术前进行血管栓塞可能有利于减少术中出血及肿瘤的整块切除。据文献报道,血管外皮瘤患者的术后复发率为76%~80%,因此术后进行辅助治疗得到认可;以长春新碱、异环磷酰胺、多柔比星、依托泊甙为基础的化疗在远处转移及复发的肿瘤治疗中开展,但并没有改善患者的预后。对中枢神经系统血管外皮瘤患者行立体定向放射治疗,肿瘤控制率在82%~93%。有研究表明,术后辅以放射治疗可使肿瘤复发的平均时间从154个月延长到254个月。大多数研究发现,术后辅以有效辐射剂量55Gy的放疗比单纯手术治疗更能减少肿瘤复发及远处转移的机会;而当不能进行外科手术治疗时,应以放疗作为首选治疗方案。
另外也有研究报道,应用酪氨酸激酶的分子靶向治疗可以使肿瘤得到更好的控制;同时建议可尝试通过抑制VEGF-VEGFR通路来控制肿瘤生长。大部分的血管外皮瘤患者在初次治疗后将会出现复发及转移,且转移大多数发生在疾病发展过程中的晚期阶段。近期研究报道,中枢神经系统血管外皮瘤患者5年生存率为85%~93%,复发率为48%~88%,远处转移率为14%~64%;通常的转移部位依次是肺、骨、肝等。血管外皮瘤患者生存率可能与放射治疗、肿瘤全部切除及病理分级有关,而复发和远处转移主要与病理改变有关。因此,应制定全身治疗方案来预防肿瘤转移,亦有必要对其进行长期随访。
综上所述,椎管内血管外皮瘤属于临床少见疾病;由于血管外皮瘤术前诊断困难、血供丰富、复发率和远处转移率高,且手术难度大,若临床上怀疑为血管外皮瘤,术前可进行血管造影评估及血管栓塞,利用现代麻醉技术结合娴熟的显微神经外科技术整块全切除肿瘤,并在术后辅以放疗,患者也可以取得较好的预后。
原始出处:
孙硕,张金凤,周辉,施辉.腰椎管内哑铃型血管外皮瘤1例并文献复习[J].临床神经外科杂志,2017,14(06):463-465.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#椎管#
36
#哑铃型#
54
#腰椎管内#
40
#椎管内#
29
#腰椎#
36
#腰椎管#
33
学习了
60