J Dent Res:牙髓干细胞介导的功能性牙髓再生
2018-11-27 lishiting MedSci原创
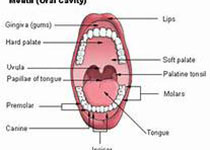
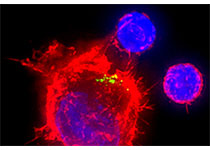
保存具有血管结构和神经组成的鲜活牙髓组织是口腔医学中最具挑战的内容之一。基于神经血管化的免疫潜力,间充质干细胞(MSC)移植在再生医疗和牙齿转化实践中展现出巨大的应用前景。实际上,基于神经棘或胶质细胞来源,牙髓间充质干细胞(包含出生后的来源于恒牙的牙髓干细胞和脱落乳牙来源的干细胞)具有独一无二的特质。并且,它们存在于神经血管龛内,具有神经发生、血管发生的潜力以及诱导神经血管的活性。
保存具有血管结构和神经组成的鲜活牙髓组织是口腔医学中最具挑战的内容之一。基于神经血管化的免疫潜力,间充质干细胞(MSC)移植在再生医疗和牙齿转化实践中展现出巨大的应用前景。实际上,基于神经棘或胶质细胞来源,牙髓间充质干细胞(包含出生后的来源于恒牙的牙髓干细胞和脱落乳牙来源的干细胞)具有独一无二的特质。并且,它们存在于神经血管龛内,具有神经发生、血管发生的潜力以及诱导神经血管的活性。基于目前牙髓再生的策略,牙髓干细胞介导的再生方法展现出令人信服的数据,它们可以原位重建具有天然牙髓的复杂组织学结构,并且具有高度有机化的生理学模式,甚至可获得新生的完整牙髓组织。更重要的是,目前临床研究强调的是通过牙髓干细胞移植以获得具有原位神经血管化的有活力的牙髓再生。在这篇综述中,作者概述了目前牙髓干细胞介导的牙髓再生的突破,突出了关键性的神经血管化成果。这种功能性的牙髓再生代表着未来再生牙髓治疗的一种革新以及治疗方向。原始出处:Sui B, Chen C, et al. Pulp Stem Cell-Mediated Functional Pulp Regeneration. J Dent Res. 2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#牙髓#
38
#功能性#
37
#牙髓再生#
39
#牙髓干细胞#
26
谢谢分享学习
92