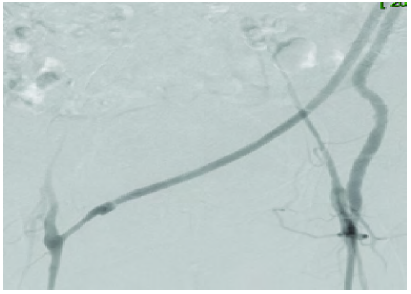
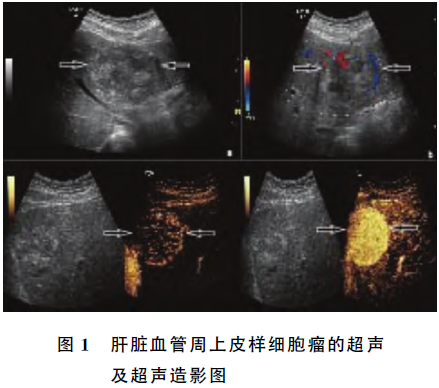
超声造影诊断搭桥人工血管狭窄1例
2019-08-25 张少云 王静 宋越 临床超声医学杂志
患者女,62岁,因“右下肢肿胀2个月余”入院。患者8年前因双侧髂总动脉和髂外动脉硬化闭塞行“左腋动脉-双股动脉人工血管搭桥术”。2个月前无明显诱因出现右下肢肿胀伴疼痛,步行后加剧。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#超声造影#
0
#人工血管#
38
#搭桥#
34
#造影#
29