Cell Mol Immunol:杜昌升教授研究组发现G蛋白Gαq参与调控多发性硬化症发生
2017-04-21 佚名 同济大学生命科学与技术学院
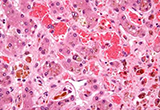
近日Cellular & Molecular Immunology(CMI)杂志在线发表同济大学生命科学与技术学院杜昌升教授、交大医学院刘俊岭教授、国家新药筛选中心谢欣教授研究组合作完成的题为“Deficiency of G protein Gαq ameliorates Experimental Autoimmune Encephalomyelitis with impaired DC-
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Gαq#
30
#Cell#
0
#G蛋白#
31
#多发性#
30
#硬化症#
27
#CEL#
25
牛,谢谢分享大牛文章
39