NEJM:贲门失弛缓症患者的螺旋状食管-病例报道
2020-04-30 MedSci原创 MedSci原创
高分辨率食管测压发现食管下括约肌的综合舒张压升高,不蠕动,与III型(痉挛性) 贲门失弛缓症相一致的痉挛性收缩。
患者为一名83岁的妇女,因进餐时出现的吞咽困难和反流,并伴有餐后胸痛,而到消化内科就诊。
几年来,她一直难以吞咽固体和液体食物,而且这种症状在就诊前的一年中已经恶化。她还报告说,去年体重减轻了9公斤。
钡盐食管图呈螺旋状(如图A所示)。上消化道内镜检查发现非蠕动性痉挛性收缩(如图B所示)和胃食管连接紧密。高分辨率食管测压发现食管下括约肌的综合舒张压升高,不蠕动,与III型(痉挛性) 贲门失弛缓症相一致的痉挛性收缩。
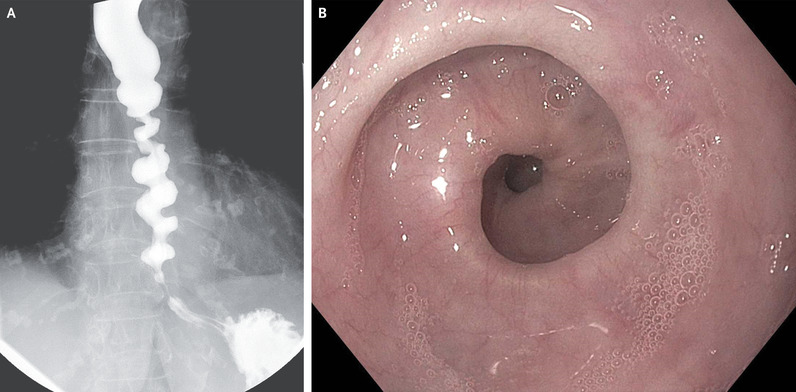
该患者拒绝内镜下肌切开术,并选择内镜下注射肉毒杆菌毒素进行治疗。治疗后5个月的随访中,她仅有间歇性吞咽困难,没有反流。
原始出处:
Samuel Han,et al.Corkscrew Esophagus in Achalasia.N Engl J Med 2020;https://www.nejm.org/doi/full/10.1056/NEJMicm1911516
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
57
#螺旋状食管#
35
#贲门#
32
#食管#
36
#贲门失弛缓症#
39
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
55