肾黏液样小管状和梭形细胞癌合并多发椎体转移一例
2019-09-04 林江南 许茂盛 临床放射学杂志
患者男,28岁。2个月前无明显诱因下出现腰背部疼痛就诊于当地医院。腰椎MRI示:胸腰椎多发椎体及附件骨质破坏,考虑恶性骨肿瘤可能,转移瘤待排除。为求进一步诊治数日后来我院就诊。患者既往无血尿,无尿频、尿急、尿痛等不适,身体状况良好。行胸椎活检术,病理免疫组织化学结果提示肾脏上皮性肿瘤转移可能性大。
患者男,28岁。2个月前无明显诱因下出现腰背部疼痛就诊于当地医院。腰椎MRI示:胸腰椎多发椎体及附件骨质破坏,考虑恶性骨肿瘤可能,转移瘤待排除。为求进一步诊治数日后来我院就诊。患者既往无血尿,无尿频、尿急、尿痛等不适,身体状况良好。行胸椎活检术,病理免疫组织化学结果提示肾脏上皮性肿瘤转移可能性大。
CT检查显示左肾上极占位影,大小约31mm×26mm,平扫呈等低密度,增强扫描皮质期轻度强化,髓质期强化较皮质期明显(图1)。MRI检查显示左肾上极见一类圆形异常信号影,T1WI呈稍低信号,T2WI呈稍高信号,DWI呈明显高信号,范围约29mm×23mm,增强扫描病灶信号欠均匀(图2、3)。附见:所见椎体内见多发结节样异常信号影,增强扫描呈环形强化(图4)。左肾上极占位,考虑恶性肿瘤。穿刺及病理:CT引导下左肾肿块穿刺活检。病理诊断:“左肾穿刺”上皮细胞来源恶性肿瘤,结合免疫组织化学,考虑黏液样小管状和梭形细胞癌(图5)。
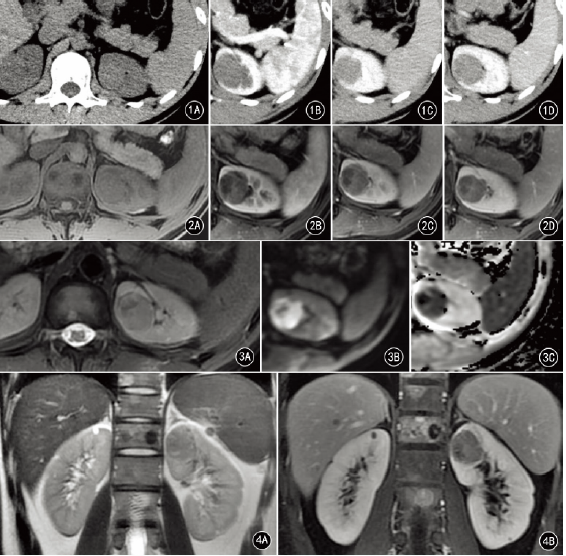
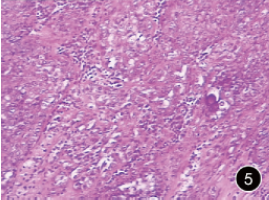
图1A~D为CT平扫、皮质期、髓质期及延迟期图像。A.示左肾上极肿块,平扫呈等低密度;B.示皮质期肿瘤外周部轻度强化,中央强化不明显;C、D.髓质期及延迟期示肿块渐进性强化;图2A~D为MRI平扫、皮质期、髓质期及延迟期图像。A.示左肾上极肿块,T1WI呈稍低信号;B.示皮质期;C、D.髓质期及延迟期示肿块渐进性强化;图3A~CA.T2WI呈稍高信号;B.DWI呈明显高信号;C.ADC呈明显低信号;图4A、BA.冠状位T2WI可见椎体多发异常信号影;B.增强扫描椎体病变呈环形强化;图5病理诊断为“左肾穿刺”上皮细胞来源恶性肿瘤(HE×100)
讨论
肾黏液样小管状和梭形细胞癌(mucinous tubular and spindle cell carcinoma,MTSCC)是一种较罕见的低度恶性肾上皮肿瘤,由Ordonez等于1996年首先报道发现。2004年WHO泌尿系统和男性生殖器官肿瘤分类中将其确定为一种新的肾细胞癌亚型。该病好发于成年女性,发病年龄17~82岁,平均53岁。多数患者无明显特殊症状,临床上常为偶然发现,部分患者可有血尿、腰痛、反复的泌尿系统感染和肾结石等表现。典型的MTSCC通常局限于肾脏,罕有淋巴结、骨和肺转移的报道。
影像学表现:CT平扫肿瘤多以等密度为主,表现为单发实性病灶,位于肾实质内,多位于肾内,少部分突出于肾实质外,密度较均匀,偶有点、片状钙化,小片出血或囊变坏死等。增强扫描皮质期强化程度较低,髓质期及延迟期病灶渐进性强化,但仍低于正常的肾实质。因此肾实质期的影像表现对于MTSCC的诊断有重要意义。MRI像上肿瘤T1WI呈等信号或低信号,T2WI信号因其内部成分不同而变化不一,多数可在T1WI及T2WI观察到肿瘤周围有环形低信号。
鉴别诊断:
(1)其他类型的肾细胞癌。透明细胞癌:该肿瘤恶性程度较高,常伴有囊变坏死、出血等,增强扫描皮质期明显强化,髓质期迅速减退,两者鉴别较易。嫌色细胞癌:平扫密度及信号一般较均匀,强化也较均匀,易出现钙化,较少发生出血、坏死、囊变,强化多出现在皮质期、髓质期,延迟期稍减退。集合管癌:平扫密度欠均匀,强化程度也不高,但其恶性程度高,常呈浸润性生长,累及肾盂、肾周,淋巴结及远处转移亦常见。乳头状癌:较易出血,而MTSCC出血较少。
(2)良性肾肿瘤。血管平滑肌脂肪瘤:CT可见脂肪密度,MRI可见脂肪信号;增强扫描为富血供,早期强化,持续时间长。嗜酸细胞腺瘤:可表现为边界清晰的实性肿块,中等强化,出血、坏死少,部分中心可见星状瘢痕和轮辐状强化。MTSCC是非常少见的低度恶性肿瘤,CT及MRI增强扫描皮质期、髓质期持续性强化,但仍低于肾实质的强化方式可能对其诊断有重要价值。由于对MTSCC的认识不足,影像学诊断较难,其准确诊断仍需依赖病理学检查。
原始出处:
林江南,许茂盛.肾黏液样小管状和梭形细胞癌合并多发椎体转移一例[J].临床放射学杂志,2018(04):585-586.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#黏液样#
34
#梭形细胞#
37
#细胞癌#
31
#椎体#
31