乳腺增生会癌变吗,到底要不要治?每个女人都该知道
2017-09-18 霍莉莉 邱天 上海中医药大学附属上海市中西医结合医院治未病科 海上名医
近年来,一些女性名人因为乳腺癌英年早逝,使得很多人“谈乳色变”。当一些女性朋友在体检报告上发现“乳腺小叶增生”的字样时,不禁担心疑惑:乳腺小叶增生是怎么回事?我怎么会得这个毛病呢?这个病会不会发展成乳腺癌?需要治疗么?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了很多先进水平
61
#乳腺增生#
41
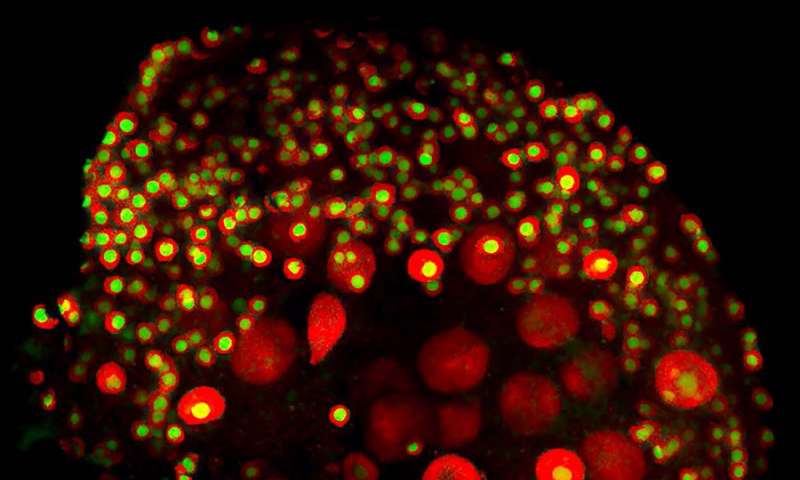
#癌变#
38
真的很棒!谢谢老师!
64
真的很棒!
62
谢谢分享.学习了
60
越来越多的乳腺疾病
58