Clin Cancer Res:基于多参数磁共振影像组学预测晚期鼻咽癌患者无进展生存期
2017-08-28 MedSci MedSci原创
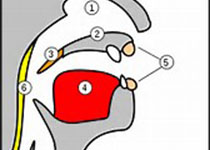
鼻咽癌是亚洲特别是中国华南地区常见的恶性肿瘤。局部复发及远处转移是治疗失败的主要原因。因此提前预测鼻咽癌患者不良预后显得尤为重要,为临床提供有益指导。近期,张水兴教授带领他的团队探讨基于磁共振影像组学(Radiomics)预测晚期鼻咽癌(III-IVb期)患者无进展生存期(Progression-Free Survival,PFS)的可行性。相关研究成果刊登在肿瘤领域权威期刊《Clinical C
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了,谢谢作者分享!
41
#磁共振#
34
#生存期#
25
#无进展生存期#
29
继续学习中谢谢
37
学习一下谢谢分享
34
谢谢分享.
49