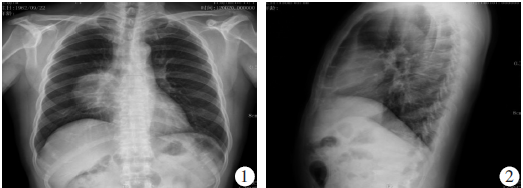
Chest:中国肺癌死亡率的空间和时间趋势
2019-08-15 xing.T MedSci原创
由此可见,亚组人群中LCMR的时空趋势差异凸显了对潜在驱动因素进行调查的必要性,尤其是对中国东部、南部和西南部的驱动因素。这些发现可能有助于卫生部分针对最需要的人群进行干预,以减轻中国的肺癌负担。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肺癌死亡率#
33
#EST#
25
#时间趋势#
33
#Chest#
33
变化的数据,学习了
65
学习了
79