Gastric Cancer:腹腔镜保留幽门胃切除术是术后胃淤滞的危险因素
2020-07-04 MedSci原创 MedSci原创
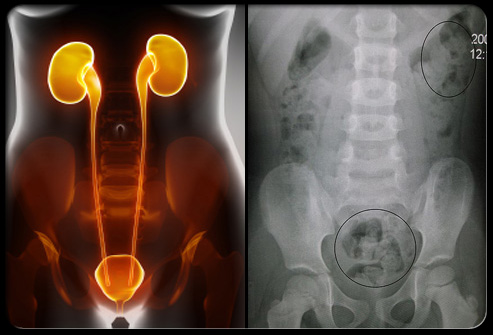
保留幽门的胃切除术是位于胃中部的胃癌的一种手术方式,目前已通过腹腔镜方法(LPPG)进行。PPG有时在术后早期病程中伴有关键问题,即胃瘀滞,因此本项研究旨在探究此手术方式是否是导致胃瘀滞的危险因素。
背景
保留幽门的胃切除术(PPG)是位于胃中部的胃癌的一种手术方式,目前已通过腹腔镜方法(LPPG)进行。PPG有时在术后早期病程中伴有关键问题,即胃瘀滞,因此本项研究旨在探究此手术方式是否是导致胃瘀滞的危险因素。
方法
该研究包括897例在2005年至2017年间接受LPPG的患者。当满足以下条件时,即定义了术后早期胃淤滞(E淤滞):上腹胀,X线摄片上剩余的胃部充盈以及饥饿时间在72小时内超过72 h术后1个月。为了评估E淤滞的长期结局,根据术后1年的RGB(残留,胃炎,胆汁)分类,将术后晚期残留食物(L-残留)在内窥镜下定义为2级或更高残留食物。
结果
胃瘀滞是术后早期过程中最常见的并发症。68名(7.6%)患者发生了胃淤滞。多因素分析确定年龄(≥61岁),糖尿病和术后腹腔内感染为危险因素。术后1年,经历淤滞的患者的相对体重比和术后血清白蛋白显着低于其他患者(P = 0.042和0.011)。在患有瘀滞的患者中,有42.5%的患者经历了L-残留。
结论
7.6%的患者发生LPPG后出现胃淤滞。年龄,糖尿病和腹腔内感染与术后胃瘀滞显着相关。
原始出处:
Ryo Takahashi. Et al. Risk factors and prognosis of gastric stasis, a crucial problem after laparoscopic pylorus-preserving gastrectomy for early middle-third gastric cancer. Gastric Cancer.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#gastric#
30
#AST#
33
#切除术#
31
#GAS#
45
#腹腔镜#
37
#胃切除#
51