CCLM: d -乳酸水平较高与肥胖青少年高浓度低密度脂蛋白的患病率有关?
2018-06-28 MedSci MedSci原创
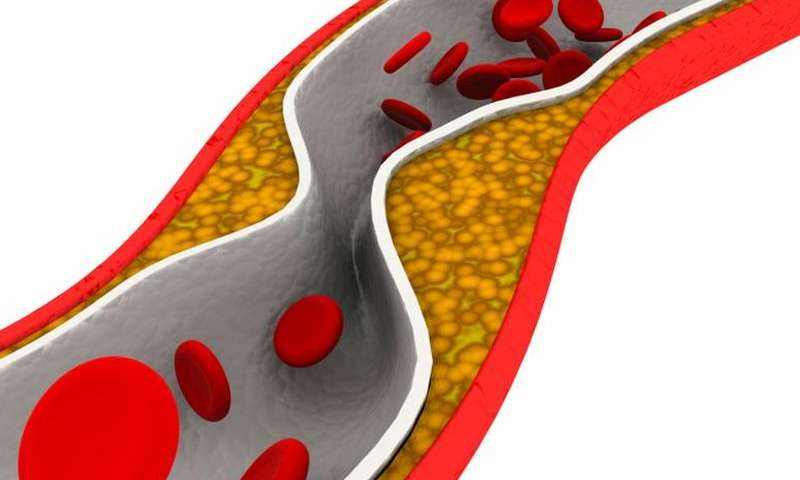
儿童肥胖与胰岛素抵抗(IR),低浓度低密度脂蛋白(sd-LDL)水平增加以及肝脏新生脂肪形成增加有关,这意味着丙糖磷酸增加可能导致甲基乙二醛(MG)及其分解代谢终产物D-乳酸盐的增加。我们假设肥胖青少年D-乳酸血清水平的增加与sd-LDL高发生率相关。 这是一项横断面研究,对30名瘦型青少年和30名肥胖青少年(16名女性和14名男性每人)研究其人体测量学特征,致动脉粥样硬化性血脂异常综合征,
儿童肥胖与胰岛素抵抗(IR),低浓度低密度脂蛋白(sd-LDL)水平增加以及肝脏新生脂肪形成增加有关,这意味着丙糖磷酸增加可能导致甲基乙二醛(MG)及其分解代谢终产物D-乳酸盐的增加。我们假设肥胖青少年D-乳酸血清水平的增加与sd-LDL高发生率相关。
这是一项横断面研究,对30名瘦型青少年和30名肥胖青少年(16名女性和14名男性每人)研究其人体测量学特征,致动脉粥样硬化性血脂异常综合征,sd-LDL(Lipoprint,Quantimetrix)和D-乳酸(动力学酶分析)。此外,还通过血流介导的扩张(FMD,通过超声)测量了内皮功能,以及从国颈动脉内膜中层厚度(CIMT,通过超声)测量了动脉损伤的程度。
结果显示,参与者的平均年龄为16.8±1.4岁。肥胖青少年的体重指数为32.7±3.8,瘦型青少年体重指数为21.8±2.1。肥胖组显示较高的D-乳酸水平:6.2±3.0比4.5±2.5μmol/ L,较高的胰岛素水平:15(9.6-23.5)比7.9(6.5-10.5)μIU/ mL; 甘油三酯(TG):1.46(1.1-1.8)对0.84(0.6-1.2)mmol / L; 非高密度脂蛋白胆固醇(NON-HDL-C):2.8±0.9比2.3±0.7mmol / L; 总胆固醇(TC)/ HDL-C)指数:2.9±0.7比2.4±0.5; TG / HDL-C指数:2.2(1.5-2.8)对1.1(0.8-1.8); %LDL-3:4.2±4.07比1.9±2.7; 更小的LDL尺寸:270.6±3对比272.2±1.1Å。D-乳酸分别与LDL-2和LDL-3(sd-LDL)正相关(r = 0.44和
r = 0.49),与LDL-1和LDL大小负相关(r = -0.48和r = -0.46)。
研究表明,肥胖青少年表现出IR和内皮功能障碍的亚临床症状。血清sd-LDL水平越高,D-乳酸水平越高。这些研究结果表明,在看似健康的肥胖青少年中,动脉粥样硬化血脂异常蛋白血症与全身MG流体之间存在关联。
原始出处:
Rodríguez-Mortera, Reyna, Higher D-lactate levels are associated
with higher prevalence of small dense low-density lipoprotein in obese
adolescents
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习,谢谢分享
68
#患病率#
23
#脂蛋白#
24
#浓度#
22
学习.谢谢分享
35
阅
66