Cancer Cell:军事医学研究院叶棋浓组揭示肿瘤Warburg 效应转录调控的新机制
2018-02-17 BioArt BioArt
恶性肿瘤不仅是一种基因病,也是一种能量代谢性疾病。即使在氧供应充分的条件下,肿瘤细胞也主要以糖酵解获取能量,称之有氧糖酵解或“Warburg效应”,这种肿瘤细胞的糖酵解异常会促进葡萄糖摄取和乳酸生成,从而有利于肿瘤的发生发展。目前,“Warburg效应”作为肿瘤的一个典型标志已被广泛认可。2011年,Robert A.Weinberg教授在Cell杂志发表综述,将肿瘤异常的代谢表型列入肿瘤十大特征

十余种编码糖酵解关键酶的基因直接负责调控Warburg效应。转录因子在调控糖酵解关键酶基因以及调控Warburg效应中发挥着直接且关键的作用。例如缺氧诱导因子(Hypoxia-inducible factor-1α, HIF-1α)、c-Myc、NF-kB、p53等。
HIF-1α是Warburg效应的关键调控因子,通过与糖酵解基因启动子上的缺氧反应元件(hypoxia-responsive elements, HRE)结合来促进糖酵解基因的表达。c-Myc能够直接转录激活编码葡萄糖转运体1 (GLUT1)和乳酸脱氢酶 (LDHA) 的糖酵解基因,并促进异常糖酵解。p53肿瘤抑制因子通过直接抑制GLUT1和GLUT4基因的转录,从而抑制葡萄搪摄取和乳酸产量。然而,目前报道的调控Warburg效应的转录因子只有少数几个,Warburg效应的转录调控机制在很大程度上仍不清楚。
北京时间农历正月初一凌晨,军事医学研究院生物工程研究所叶棋浓课题组在Cancer Cell杂志上以Articles的形式发表了题为“Transcriptional Regulation of the Warburg Effect in Cancer by SIX1”的研究论文,该研究发现SIX1是一个新的调控Warburg效应的关键转录因子,SIX1调控糖酵解的功能够直接被miR-548a-3p抑制,首次将miR-548a-3p/SIX1轴与Warburg效应和肿瘤生长联系起来,并阐明了相关作用机制。
转录因子SIX1是器官形成的关键调控因子,SIX1敲除的小鼠胚胎存在着多器官发育缺陷、较野生型小鼠个头小的现象,而且SIX1敲除小鼠在出生后不久就死亡。SIX1在多种肿瘤中高表达,例如乳腺癌、前列腺癌、肝癌、结直肠癌等。SIX1高表达的患者临床预后较差。SIX1能够促进肿瘤生长和转移。然而,SIX1是否调控肿瘤Warburg效应未见报道。
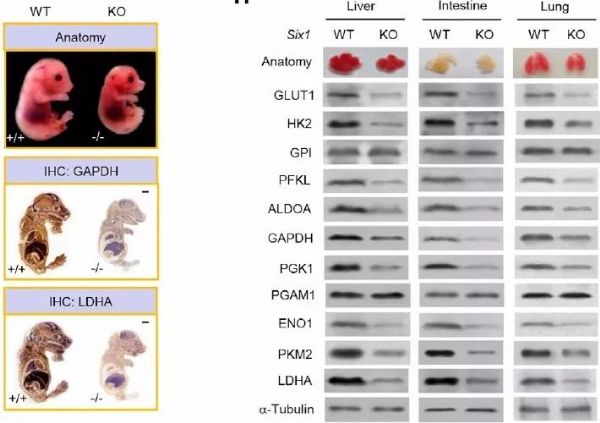
在最新的这项研究中,研究人员利用稳定敲低SIX1的乳腺癌ZR75-1细胞与对照细胞进行转录组测序(RNA-seq),结合实时定量PCR技术,发现SIX1能够影响糖酵解通路。接下来,在SIX1 Knock Out(KO)的乳腺癌、SIX1 Knock Down(KD)的肝癌细胞系中均证实了SIX1能够促进GLUT1、HK2、PFKL、ALDOA、GAPDH、PGK1、ENO1、PKM2、LDHA 九个糖酵解关键基因的转录和表达。SIX1基因回补实验也证实了这一点。在SIX1 KO小鼠胚胎成纤维细胞(MEFs)、KO小鼠胚胎以及胚胎中分离出的肝、肠、肺等组织中观察得到相似的结果(下图)。以上均提示,SIX1是一个调控糖酵解基因转录与表达的关键因子。那么,SIX1是如何调控这些糖酵解基因的转录呢?
由于之前报道的ChIP-seq和ChIP-on-chip数据结果提示,SIX1与DNA结合的特征模序为TCAG/TG,数据库结果也显示SIX1直接结合于6个糖酵解基因(PFKL, ALDOA, PGK1, ENO1, PKM2和LDHA)的启动子上。为了研究SIX1如何具体调控糖酵解基因的转录,研究人员寻找了受调控的糖酵解基因启动子上游近3 kb的区域中含有SIX1结合位点的序列,并构建了相应的启动子。利用荧光素酶活性以及染色质免疫共沉淀(ChIP)试验,证实了SIX1调控糖酵解基因的转录是通过结合于它们的启动子来实现的。
由于转录因子与组蛋白修饰酶之间的相互作用对于基因转录调控至关重要,且组蛋白乙酰化通常与基因转录激活密切相关。为了研究SIX1如何激活糖酵解基因的转录,研究人员利用免疫共沉淀结合质谱方法筛选出了两个与SIX1相互作用的组蛋白乙酰转移酶—HBO1与AIB1。利用HBO1和AIB1 KO、KD细胞发现,SIX1调控糖酵解基因的表达需通过与HBO1和AIB1的相互作用实现。接下来,研究人员研究了SIX1如何通过HBO1和AIB1调控糖酵解基因的分子机制。ChIP结果显示,SIX1促进糖酵解基因的转录是通过HBO1介导的H4K5乙酰化和AIB1介导的H3K4乙酰化实现的。
那么,SIX1的上游调控因子是什么呢?研究人员筛选了靶向SIX1的miRNA,结果发现miR-548a-3p能够直接且特异地靶向SIX1。miR-548a-3p抑制SIX1表达,并抑制糖酵解基因的表达。利用SIX1 KO细胞检测发现,miR-548a-3p通过SIX抑制糖酵解基因的表达。
miR-548a-3p/SIX1轴对肿瘤细胞糖酵解的功能产生什么影响呢?细胞学实验证明,miR-548a-3p/SIX1轴调控了肿瘤细胞的葡萄糖摄取、丙酮酸、乳酸及ATP水平、细胞外酸化率(ECAR)以及细胞有氧呼吸消耗速率(OCR)。SIX1需通过HBO1和AIB1发挥以上功能。miR-548a-3p/SIX1轴通过调节糖酵解影响细胞生长。由于缺氧是实体肿瘤最显着的特征,研究人员进一步发现,miR-548a-3p被缺氧抑制,SIX1被缺氧诱导,miR-548a-3p/SIX1轴在缺氧条件下仍发挥调节肿瘤糖酵解和细胞生长作用。
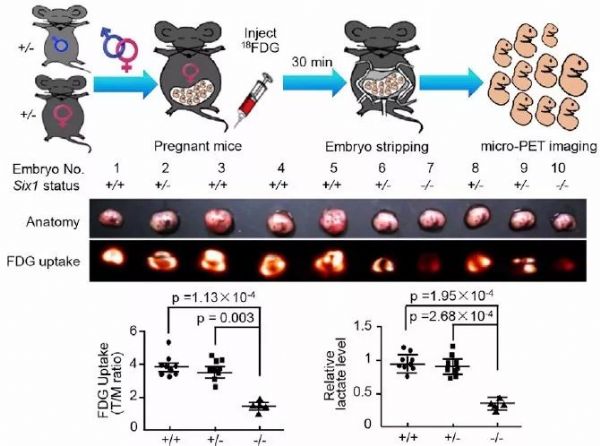
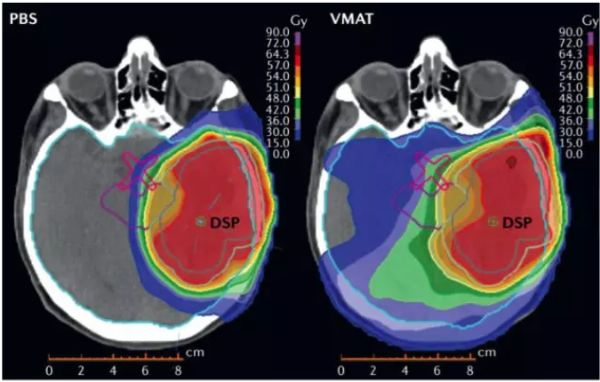
随后,研究人员利用18FDG标记的小动物PET技术显像发现,miR-548a-3p通过SIX1调控裸鼠异种移植瘤的糖摄取能力,而SIX1通过HBO1和AIB1调控糖摄取能力,更重要的是,miR-548a-3p/SIX1轴介导的糖酵解对于肿瘤细胞的生长是关键的。为了验证生理条件下miR-548a-3p/SIX1轴与糖酵解之间的相关性,研究人员利用小动物PET技术对胎鼠进行显像,结果发现,SIX1 KO胎鼠与野生型、杂合子胎鼠相比糖摄取与乳酸水平明显降低(下图)。
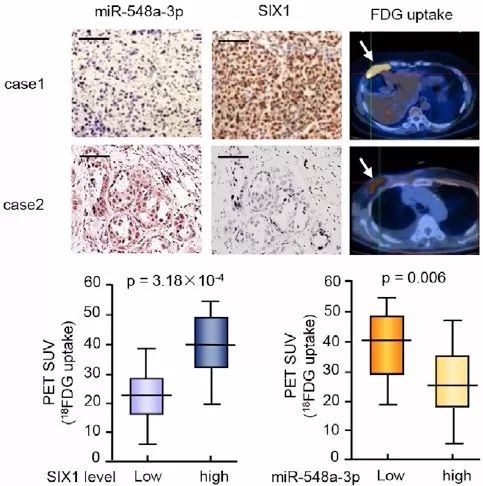
miR-548a-3p/SIX1轴在临床上有什么意义呢?首先,研究人员比较了临床上接受PET-CT检测的乳腺癌患者肿瘤摄取与miR-548a-3p、SIX1表达的关系,结果发现,肿瘤摄取高的患者miR-548a-3p表达低、SIX1表达高(下图)。对更多乳腺癌患者标本进行检测发现,miR-548a-3p表达与PGK1、LDHA等糖酵解基因成负相关、SIX1与糖酵解基因表达成正相关。TCGA数据库与Oncomine数据库分析也证实了上述相关性。另外,miR-548a-3p表达高的患者预后较好。
有意思的是,肿瘤中存在SIX1 Q177R突变,因此研究人员猜想该肿瘤相关突变体是否与糖酵解基因表达有关。利用SIX1 KO 肿瘤细胞系与KO MEF,研究人员分别转入野生型、突变体表达载体,检测结果显示,与野生型相比,SIX1 Q177R突变体进一步促进了HK2、GAPDH、PKM2和LDHA基因表达,葡萄糖摄取、丙酮酸、乳酸、ATP水平进一步升高,从而促进了肿瘤生长。
综上,这项研究阐明了在缺氧条件下,miR-548a-3p表达抑制,其下游靶基因SIX1活化,活化的SIX1通过与组蛋白乙酰转移酶HBO1和AIB1相互作用,激活了多个糖酵解基因的转录与表达,进而影响调控糖酵解的能力,最终促进细胞恶性转化及癌症发生(下图)。
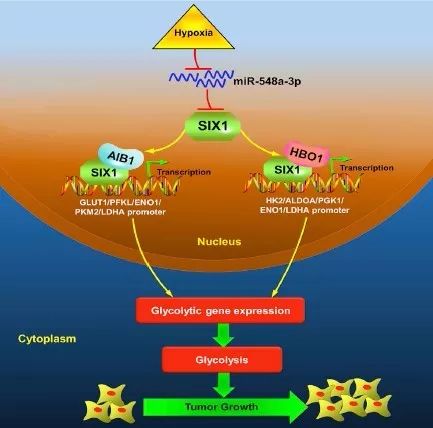
MiR-548a-3p/SIX1轴调控Warburg效应和肿瘤生长
本研究首次发现了在肿瘤Warburg效应中起重要调控作用的miR-548a-3p/SIX1轴,该轴线将Warburg效应与肿瘤紧密联系起来,为开发新的抗癌药物提供了候选靶标,也为评估恶性肿瘤的预后提供有用信息。
据悉,本研究的通讯作者为叶棋浓研究员和徐小洁副研究员,论文的第一作者为李玲博士和梁迎春博士后。该研究得到了中国人民解放军总医院刘阳主任医师、李瑛主任医师,中科院苏州生物医学工程技术研究所高山研究员, 中国人民解放军307医院王涛副主任医师等的大力支持。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#转录#
31
#Cell#
19
#CEL#
27
#cancer cell#
34
#转录调控#
37
肯定是一种能量代谢病.而且是高代谢率.
60
军事医学研究院叶棋浓的研究.
54
#医学研究#
26
学习了谢谢分享!!
63
学习了.谢谢分享.
56