ECMO辅助下罕见巨大气管内肿瘤切除术麻醉管理一例
2019-04-03 朱小兵 吴论 伍嘉艳 临床麻醉学杂志
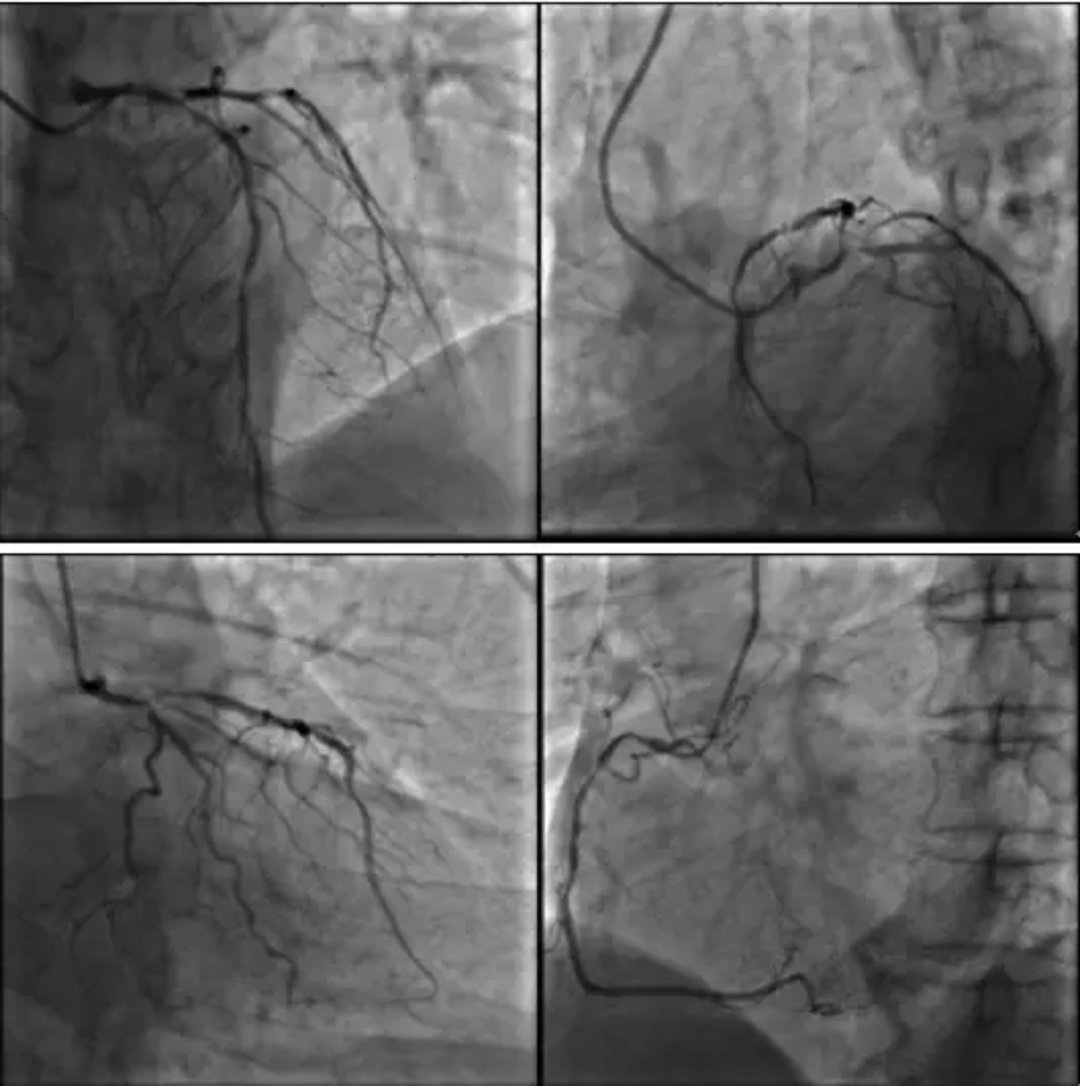
患者,女,53岁,158 cm,54kg,因“反复咳嗽气促2年,加重4月”入院。术前一般情况可,未见明显口唇紫绀,术前BP142/71mmHg,HR70次/分,近20d来,患者行走60~70m出现气促,无明显诱因下静息状态下出现憋喘,夜间睡眠无憋醒史。术前诊断:气管肿瘤:性质待诊;高血压2级。拟在全身麻醉下行“气管内肿瘤切除、气管重建术”。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#罕见巨大#
36
#切除术#
33
#CMO#
40
紧急情况下建立ECMO,熟练的需要几分钟
76
#肿瘤切除#
51
#罕见#
29