临床研究者指南:临床研究的可靠性及一致性
2016-06-13 谭玉勇 王东 译 Gut
临床医生及研究人员每天都面临着测量多种指标的挑战。从疗效和疾病活动度评价,到确诊及前沿诊断手段的革新。测量结果的有效性、可重复性及可靠性对临床工作的各个方面都是至关重要的。初看上去,有效性、可重复性、可靠性和一致性似乎很相似,然而在研究的设计、执行以及方法学和统计学分析等方面,这些概念有着本质的区别。Alvan Feinstein发现了这个问题,并提出了临床计量学的概念,即“研究临床医学中计量问题
临床医生及研究人员每天都面临着测量多种指标的挑战。从疗效和疾病活动度评价,到确诊及前沿诊断手段的革新。测量结果的有效性、可重复性及可靠性对临床工作的各个方面都是至关重要的。初看上去,有效性、可重复性、可靠性和一致性似乎很相似,然而在研究的设计、执行以及方法学和统计学分析等方面,这些概念有着本质的区别。Alvan Feinstein发现了这个问题,并提出了临床计量学的概念,即“研究临床医学中计量问题的方法学学科”。临床计量学的概念并非一个新概念,相反,它被认为是心理测量学的一个分支。这也是本文的核心是基于健康状态测量仪器选择的共识标准(Consensus-based Standards for the selection of health Measurement Instruments,COSMIN)来倡议的原因。
(1)对可靠性及一致性的关键概念进行综述;
(2)概述可靠性及一致性相关可用的统计学工具;
(3)提出一个基于可用核查表来分析或报告高质量可靠性或一致性研究的方法。
为此,PubMed有一种搜索引擎用以识别可靠性及一致性研究相关的相关文献,本文已纳入这些相关文献。该引擎不是为系统评价而设计的,而是为当前这种叙述性综述如何选择参考文献提供方向。
COSMIN倡议是一个多学科的国际性共识,旨在建立一个用以评价测量工具性能、研究方法学质量、研究设计及选用合适的统计分析方法的标准。由于测量指标复杂,该倡议一开始主要侧重于患者报告的健康相关结局指标(health related patient-reported outcomes,HR-PRO),然而这些概念也用于其他类型的结局指标,这在随后的内容中将会提到。需要说明的是,Mokkink等对HR-PRO的定义为“患者对自身健康状况的任何方面的自评结果,也就是说,不包括医生或其他人解释后患者的回答”,例如包括自填问卷或计算机管理的调查问卷。
COSMIN对测量工具的以下三个主要维度进行评价:可靠性、效度及反应性。每一维度均有数个帮助评价该领域的指标,这些指标相互联系。尽管所有维度对一个新工具的评价都十分重要,本综述旨在给可靠性维度的使用提供指导,因为这一维度在胃肠道研究中经常涉及,且与诊断试验相,研究者们对此知之甚少。如想了解其他维度及其评价的详细内容,可阅读相关参考文献。
采用与Gisev等提出的相似方案,但须符合COSMIN倡议核查表、可靠性研究质量评价表(quality appraisal of reliability studies,QAREL)和可靠性及一致性研究报告指南(guidelines for reporting reliability and agreement studies,GRRAS),这样研究者才能符合推荐出版指南的要求(图1)。同时提出了一些步骤,以指导作者按顺序完成论文写作。
基于以下两个原因,本文仅提供有限的数学公式。一是太多公式可能会吓坏大多数不熟悉统计学知识的读者;其次,只要使用正确,现有的统计学软件能直接得出结果。所以,每节之后会做一个总结,说明该使用何种方法,并为感兴趣读者提供大量参考书籍,同时举例说明STATA软件的相关操作命令(StataCorp. 2011. Stata Statistical Software: Release V.12. CollegeStation,Texas, USA: StataCorp LP)。此外,本文不会对诊断准确性研究(灵敏度、特异度)的方法学进行评价。
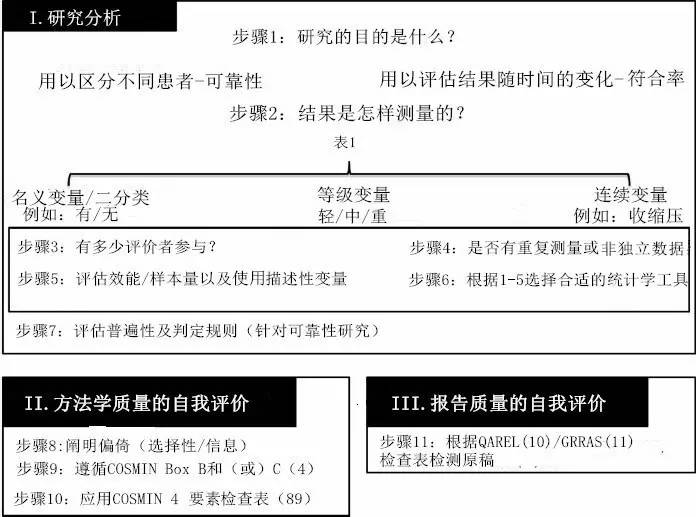
图1.分析和报告可靠性及一致性研究的分方法
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#一致性#
25
#研究者#
32
值得探讨这个问题
109
目前很多临床研究需要重视这个问题
107
学有所用
160
有点用
98