Cancer Cell:重磅来袭!结直肠癌临床基因组新突破!
2018-01-13 michael,Juka 转化医学网
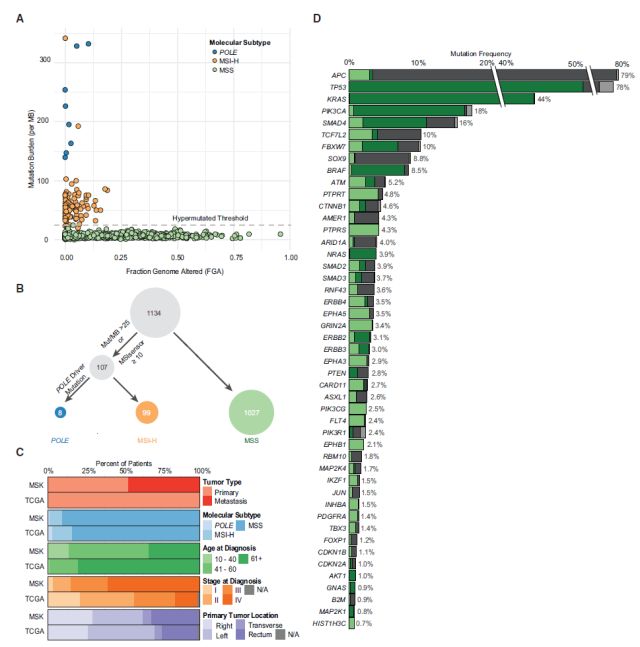
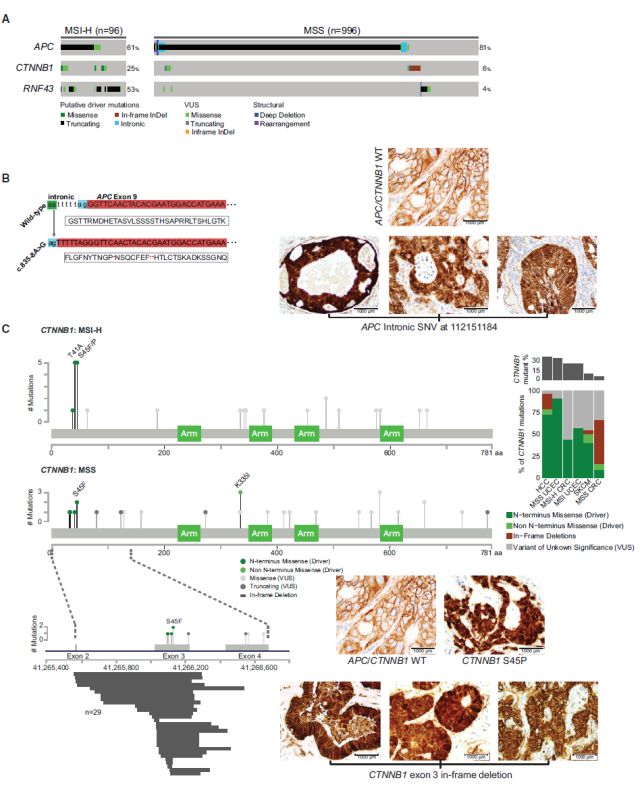
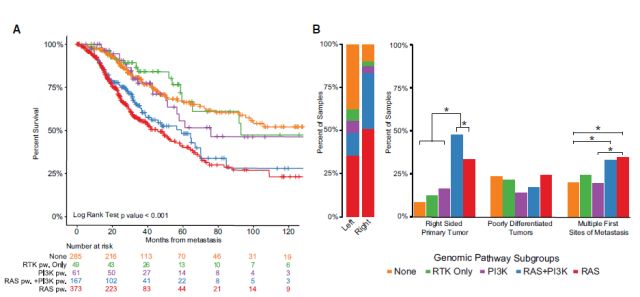
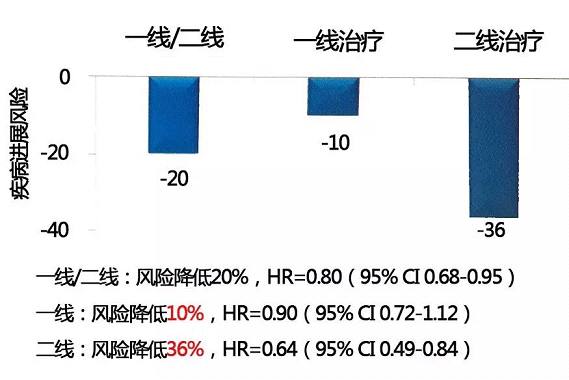
转移性结肠直肠癌(mCRC)在临床上存在异质性,但是这种可变性的基因组基础尚不明确。最近的研究结果表明,发生在右侧和左侧微小稳定型CRC不同的肿瘤产生通路可能会是产生临床差异的基因基础。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新突破#
24
#CEL#
27
#Cell#
15
#cancer cell#
26
#结直肠#
26
#重磅#
25
好文章.学习了.
54