NEJM:重度二尖瓣狭窄-病例报道
2018-07-19 xing.T MedSci原创
该患者接受了机械假体更换二尖瓣和主动脉瓣术。在为期6个月的随访中,他对身体活动只有轻微的受限(纽约心功能分级为II级)。
患者为一名47岁的男性,因急性劳累性呼吸困难不断恶化6个月而被送往急诊。他最近从洪都拉斯移民并且从小就有过心脏手术史,但最初的诊断和已经进行的具体手术尚不清楚。
体格检查显示右侧胸骨旁隆起,可听到S1心音,上胸骨边缘的中早期收缩期射血杂音(2/6级),以及心尖处的低音舒张隆隆声。心电图显示心房扑动具有可变的房室传导。
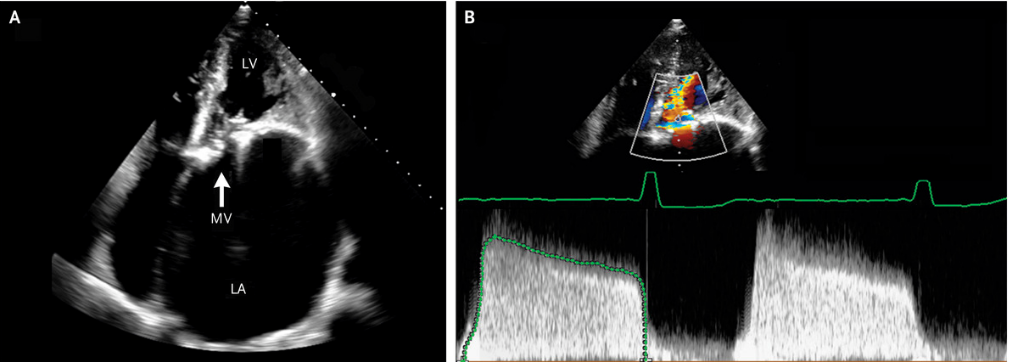
经胸超声心动图显示中度主动脉瓣狭窄(计算瓣膜面积为1.3cm2)和非常严重的二尖瓣狭窄(计算的瓣膜面积为0.5cm2)(如图A; LA表示左心房,LV左心室和MV二尖瓣)。左心房扩大,心房容积指数为每平方米364毫升(正常值<35)。彩色血流多普勒图像(如图B,上半部分)和连续波多普勒血流模式(如图B,下半部分)显示舒张期间的狭窄二尖瓣。连续波多普勒流动模式描绘了流速(垂直轴)和时间(水平轴)。传递流速的缓慢下降反映了左心房压力降低的非常缓慢,以及二尖瓣狭窄中发生的左心室舒张压的缓慢增加。平均透射梯度为14mmHg(正常值<3)。
该患者接受了机械假体更换二尖瓣和主动脉瓣术。在为期6个月的随访中,他对身体活动只有轻微的受限(纽约心功能分级为II级)。
原始出处:
Tasnim F. Imran, et al.Severe Mitral Stenosis.N Engl J Med 2018;https://www.nejm.org/doi/full/10.1056/NEJMicm1715321
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#重度二尖瓣狭窄#
33
#二尖瓣狭窄#
55
#二尖瓣#
0
好好文献学习了
56
学习了
72
二尖瓣狭窄治疗方案
62