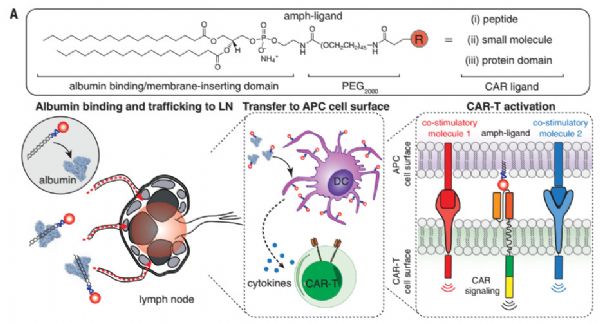
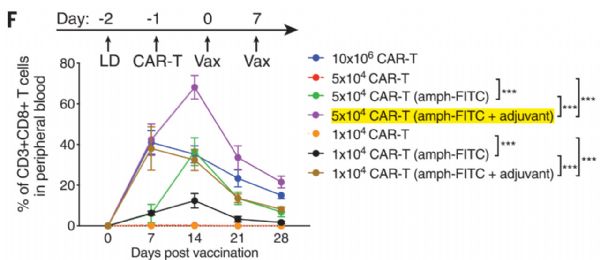
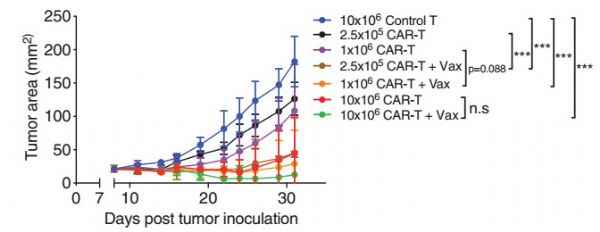
Science:MIT科学家发明两亲疫苗,大幅提高CAR-T抗癌活性,将60%小鼠肿瘤完全清除
2019-07-17 奇点糕 奇点网
2017年7月,美德两个科学家团队分别发布了开天辟地式的研究成果,他们首次利用抗癌个性化疫苗在黑色素瘤患者中大获成功,展示了癌症疫苗在癌症治疗领域的巨大潜力。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MIT#
29
#CAR-#
24
#SCIE#
27
学习了很有用不错
64
学习了
61
好
79