Lung Cancer:Nivolumab可以作为轻度IIPs的NSCLC患者的有效疗法
2020-07-28 MedSci原创 MedSci原创
研究已证实nivolumab可有效治疗转移性非小细胞肺癌(NSCLC)。肺炎是一种潜在的危及生命的免疫相关不良事件。特发性间质性肺炎(IIP)患者发生肺炎的风险较高,常被排除在临床试验之外。此外,到目
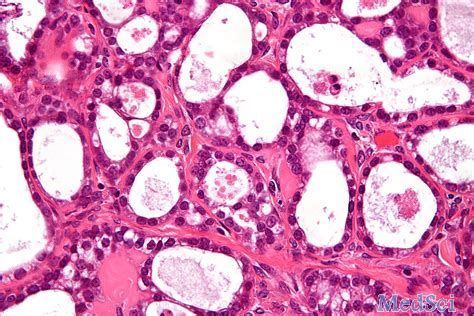
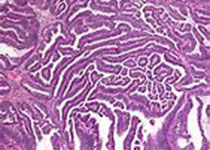
研究已证实nivolumab可有效治疗转移性非小细胞肺癌(NSCLC)。肺炎是一种潜在的危及生命的免疫相关不良事件。特发性间质性肺炎(IIP)患者发生肺炎的风险较高,常被排除在临床试验之外。此外,到目前为止,还没有针对既往治疗过的NSCLC患者进行多中心前瞻性试验。为此,我们进行了一项多中心、开放标签的单臂II期试验,以评估nivolumab在轻度IIP的NSCLC患者中的疗效和安全性。
纳入既往治疗过的、无法手术的轻度IIP的NSCLC患者。轻度IIP定义为预测生命力至少80%,且胸部高分辨率计算机断层扫描可能存在通常的间质性肺炎(UIP)或与UIP模式不一致。主要终点是6个月PFS率,次要终点是该疗法的安全性。
结果显示,18名患者参加了这项试验。6个月PFS率为56%,反应率为39%,疾病控制率为72%。没有发生治疗相关死亡。观察到1例药物相关的3/4级非血液学事件(3级神经毒性)。两名患者有2级肺炎,经皮质激素治疗后好转。
综上所述,该研究结果表明,Nivolumab可以作为轻度IIPs的NSCLC患者的有效疗法。
原始出处:
Daichi Fujimoto, Makiko Yomota, et al., Nivolumab for advanced non-small cell lung cancer patients with mild idiopathic interstitial pneumonia: A multicenter, open-label single-arm phase II trial. Lung Cancer. 2019 Aug;134:274-278. doi: 10.1016/j.lungcan.2019.06.001.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SCLC患者#
25
#mAb#
0
#NIV#
26
#iPS#
33
#NSCLC患者#
32
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
44