不一样的消化道出血
2017-10-29 MedSci MedSci原创
“梅斯医生”,一款强化医学继续教育效果的产品,改版后全新上线了!它将将带给你更好的体验与更多的惊喜!
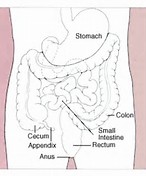
引起消化道出血的疾病有很多,如溃疡、息肉、恶性肿瘤、感染等。那么今天的病例是属于哪种呢?
病史:
患者女,56岁,4年前无明显诱因下出现黑便,每次量200g,软、成形,每天解一次,偶伴头晕, 无腹痛, 当时未予重视,未经诊治。
2 个月前头晕加重,偶有晕厥, 于当地医院就诊, 查Hb 48g/L , 胃镜示“ 胃窦出血糜烂性胃炎”, 肠镜示“ 慢性结肠炎”。予止血、输血等治疗后,头晕次数减少,但仍有黑便。期间曾行骨髓检查,提示缺铁性贫血。为进一步诊治就诊于我院。患者自发病以来精神饮食睡眠较差,二便正常。
查体:
患者神志清楚, 生命体 征平稳,皮肤、巩膜明显苍白, 浅表淋巴结未及肿大,心肺听诊无殊,腹平软,剑突下轻压痛,未及反跳痛,肝脾肋下未及,四肢双下肢无水肿直肠指诊无殊。
辅助检查:
胃镜:胃窦部见多处黏膜表浅隆起糜烂,有散在出血点, 表面有 渗出,存在胃窦血管扩张可能
超声胃镜:病灶处胃壁黏膜及黏膜下层增厚, 回声偏低, 其余各层未见异常
胶囊内镜:胃窦糜烂出血, 小肠未见明显出血病灶
外科手术术中见:胃窦部黏膜水肿, 毛 细血管扩张, 触之易渗血。
血常规:WBC 3.9*10 9 /L、N 0.6、RBC 2.6*10 12 /L、HB 44 g/l
胃镜活检病理:( 胃窦) 慢性中度浅表性胃炎、黏膜固有层见扩张迂曲血管
术后活检病理:( 胃窦部)可见黏膜下层大量厚薄不一的 扩张血管。
其他:大便潜血+、血清铁蛋白2.9 ug/l、肝肾功能、凝血功能、肿 瘤标志物检查未见异常、抗核抗体、抗中性粒细胞胞浆抗体 阴性、血清胃泌素正常
通过上面的信息,你们明白这个患者长期黑便的原因了吗?
详情尽在梅斯医生上,您可以在这里体验模拟诊疗。
下载链接:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












选题切合热点.研究价值明显
62
好资料学习了!
56
学习了.有意思
60
谢谢分享.学习了
66
#消化道#
24
明白了吗你们?请教教我
41
学习了好资料!
27
已学习并已分享
28
学习了提高了.
28