【一般资料】
患者,女,45岁
【主诉】
因“发现子宫肌瘤6个月,近期增大”于2017年3月6日收入院。
【体格检查】
妇科检查:外阴发育正常;阴道通畅;黏膜皱襞滑润,伸展良;宫颈表面光滑;子宫后位,略大于正常,表面不平,活动尚可。子宫偏右侧触及约4.0cm×4.0cm大的囊实性包块,无触痛,活动欠佳。双侧附件区未触及异常。
【辅助检查】
妇科彩超示:子宫后位,5.4cm×6.0cm×4.9cm,宫腔线清;内膜1.4cm,回声不均;宫腔内见0.9cm×0.4cm稍强回声,宫壁回声不均匀;肌层见少量点状强回声,子宫前后壁见多个低回声结节,最大位于前壁0.7cm×0.5cm,右侧壁近峡部外见4.4cm×3.7cm以实性为主的囊实混合性包块;左卵巢正常大,回声欠均,右卵巢未显示;双附件未及明显包快。CDFI:未见异常血流信号。盆腔积液深2.0cm。超声诊断:子宫多发肌瘤(合并囊性变)?子宫内膜息肉?
【初步诊断】
子宫肌瘤?子宫内膜息肉?
【治疗】
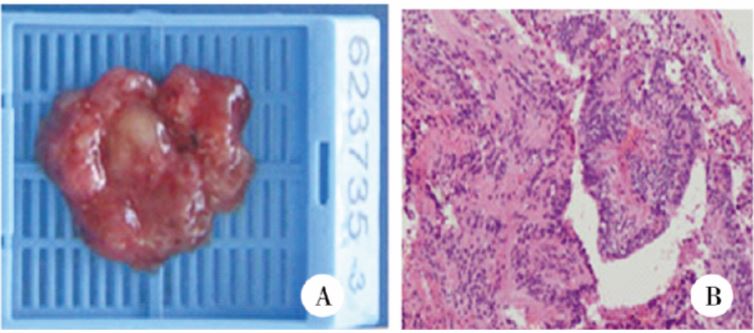
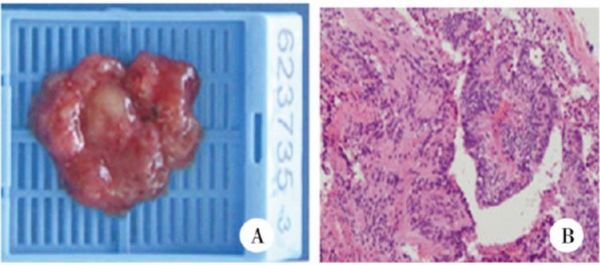
与患者及家属沟通后决定于2017年3月8日行手术治疗。术中行宫腔镜检查术,将子宫内膜息肉完整切除。腹腔镜下探查见:子宫后位,体积稍大,于右侧阔韧带方向凸出一大小约为4.0cm×4.0cm肿物,凸起程度未超过右侧圆韧带,膀胱反折腹膜稍隆起,表面光滑无粘连,双侧输卵管卵巢未见明显异常。与家属沟通后行腹腔镜下子宫阔韧带肿物切除术,剥除肿物过程中包膜破溃,有烂肉样组织溢出。肿物与子宫右侧壁界限不清。将烂肉样组织送快速病理,病理回报:(子宫肌瘤)内见异型腺体,不能除外腺癌,待石蜡切片最后确定。建议手术切除全子宫及双侧输卵管、卵巢,家属拒绝切除全子宫及双侧输卵管、卵巢。术中切除肿瘤组织,待常规病理回报后再行进一步治疗。2017年3月10日术后常规病理回报:分泌型宫内膜,局部呈息肉样改变,(子宫阔韧带肿物)恶性肿瘤,结合免疫组化染色及形态学特征考虑为室管膜瘤。北京协和医院病理会诊:(子宫阔韧带肿物)病史符合室管膜瘤,建议二次手术。2017年3月15日行扩大型全子宫切除术+双侧输卵管切除术+双侧卵巢切除术+盆腔淋巴结清扫术+恶性肿瘤病灶清除术。巨检:子宫右侧阔韧带方向凸出一囊实性肿物,大小4.0cm×4.0cm,切面灰白,糟脆,似烂肉样。镜检:瘤细胞密集排列,细胞大小较一致,细胞核呈圆形或椭圆形、深染,胞浆淡染,瘤细胞围绕中央孔呈特征性室管膜菊形团结构(图1)。免疫组化:ER(阳性率90%)、PR(阳性率90%)、P16(部分+)、Ki67(阳性率20%)、P53(-)、CK(AE1/AE3)(局部弱+)、Vimentin(+)、calretinin(-)、EMA(部分+)、α-inhibin(-)、CK7(-)、GFAP(+)、CD10(-)、PAX-8(+)、S-100(部分+)。2017年3月21日病理回报:子宫肌壁及浆膜面:室管膜瘤,浸润子宫肌壁及右侧宫旁组织,肿瘤内有出血,周围纤维组织增生;右侧输卵管管壁内及周围组织、卵巢周围组织内有浸润;右侧卵巢内见多个扩张卵泡,未见肿瘤浸润;左卵巢及输卵管未见著变,子宫多发平滑肌瘤,(右宫旁肿瘤病灶)内见少量肿瘤成分,有出血及炎细胞浸润;右侧闭孔淋巴结见肿瘤转移(2/10),余盆腔淋巴结未见转移。病理学诊断:子宫阔韧带室管膜瘤并子宫肌壁及浆膜面及右侧输卵管及右侧闭孔淋巴结转移。
【讨论】
室管膜瘤是起源于室管膜细胞及室管膜下胶质层的肿瘤,是中枢神经系统中一种特征性的胶质细胞肿瘤,占原发性中枢神经系统肿瘤的2%~9%。发生部位主要为与室管膜相近部位的颅内或脊髓内,发生于颅外或脊髓外者较罕见,最常见于骶尾部,其他发生部位包括卵巢、纵膈、子宫韧带、子宫直肠间隙和网膜等。发生于子宫韧带者加上本例仅8例。患者发病年龄13~66岁,包括阔韧带6例,卵巢系膜、宫骶韧带各1例。患者主要症状为下腹部疼痛,其次是腹部包块,常发生于单侧,且右侧多见,仅1例发生于左侧,瘤体大小不一,直径约2~14cm,呈囊实性或囊性。实性区域可有出血、坏死,切面灰白,质脆,似鱼肉样。镜下观察:子宫阔韧带室管膜瘤与中枢神经系统室管膜瘤组织学特点类似,瘤细胞大小较一致,瘤细胞的胞浆突起围绕血管形成假菊形团结构或瘤细胞围绕中央孔呈现特征性的室管膜真菊形团结构。免疫组化:与中枢神经系统室管膜瘤相比,子宫阔韧带室管膜瘤同样表达GFAP、vimentin及S-100,但前者不表达ER、PR,后者ER、PR高表达。阔韧带室管膜瘤较罕见,临床易误诊,术中快速病理易诊断为分化较差的腺癌。鉴别诊断:(1)卵巢生发上皮来源肿瘤,如浆液性腺癌,无假菊形团结构及血管周围无核区,免疫组化上皮标记物呈阳性,GFAP及S-100呈阴性。(2)颗粒细胞瘤:肿瘤细胞体积小,核深染,常可见核沟,瘤细胞环状排列形成Call-Exner小体,细胞核呈离心性排列,但小体中央缺乏血管且无明显的无核细胞区出现;免疫组化颗粒细胞瘤α-Inhibin阳性,GFAP阴性;而室管膜瘤α-Inhibin阴性,GFAP阳性。(3)平滑肌瘤:无假菊形团结构及血管周围的无核区,免疫组化表达SMA及desmin,不表达GFAP。(4)阔韧带腺肌瘤:由子宫内膜组织和增生的平滑肌组织构成,细胞无异型性。免疫组化染色:子宫内膜腺上皮及间质细胞表达ER、PR,间质细胞表达Vimtin、CD10,平滑肌细胞表达SMA,不表达GFAP。以手术切除为主,预后较好。综上,阔韧带室管膜瘤可依靠GFAP染色明确诊断。阔韧带室管膜瘤罕见,且缺乏长期随访资料,因而对其生物学行为的研究数据不足。已报道的8例阔韧带室管膜瘤(包括本例)中,3例初次手术时已出现腹腔播散性转移。阔韧带室管膜瘤的生物学行为符合低度恶性,可有多次手术机会。阔韧带室管膜瘤的预后优于中枢神经系统室管膜瘤,术后辅以放疗、化疗可延长生存期甚至可长期存活。本例患者术中已出现淋巴结转移,属于晚期病例,术后辅以化疗,随访至今患者情况良好,但仍需继续随访。
原始出处:
陈燕如, 蔺军敏, 李晶,等. 子宫阔韧带室管膜瘤1例及文献复习[J]. 现代妇产科进展, 2017, 26(12):956-957.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#管膜瘤#
36
#韧带#
20
#室管膜瘤#
23
#室管膜瘤#
35