Cancer Cell亮点:洪明奇团队开发新方法提高PD-L1阳性检出率
2019-07-28 兮 BioArt
近年来,免疫疗法已发展为癌症治疗的重要策略,而抗PD-1/PD-L1的癌症免疫疗法在经过诸多研究检视与临床试验后已广受认可,成为目前最主要的治疗方式之一,其在许多种癌症治疗上引领许多革命性的进展。
特异性抗PD-1或抗PD-L1的数株单克隆抗体,已获得美国食品和药物管理局 (FDA) 批准用于非小细胞肺癌,头颈部鳞状细胞癌,肾细胞癌,尿路上皮癌,黑色素瘤,以及经典霍奇金淋巴瘤的一线或二线治疗。然而抗PD-1/PD-L1作为单一性疗法并非对于所有的癌症病患都能有正向疗效,一般而言平均其对20-40%的患者能产生显着的治疗功效。因此,如何筛选出适合抗PD-1/PD-L1免疫疗法的病人接受治疗,而使病况获得缓解甚至痊愈是至关重要的课题。
2019年7月18日,台湾中国医药大学洪明奇教授团队(共同一作为李恒焕博士与王盈乃博士)在Cancer Cell杂志上发表文章Removal of N-Linked Glycosylation Enhances PD-L1Detection and Predicts Anti-PD-1/PD-L1 Therapeutic Efficacy,揭示了以糖苷内切酶去除糖基化的崭新方法,从而增强PD-L1检测而帮助筛选适当的肿瘤患者接受免疫疗法。
理论上,检测病人癌组织中PD-L1量来判断其是否适合抗PD-1/PD-L1免疫疗法是很合理且直接有效的做法,目前也已获得美国食品和药物管理局 (FDA) 批准而被应用在临床治疗检测上。但长期以来根据临床试验与研究的结果,PD-L1的检测量能否与病人接受抗PD-1/PD-L1疗法得到正向疗效而存在正相关性还未能有清楚的定论,因为其中广泛地存在一个矛盾而未解的现象:根据目前的PD-L1检测方法,存在10-20% PD-L1的阴性患者,在几项独立的临床试验中对于抗PD-1/PD-L1治疗仍呈现正向反应,这个事实明显有悖于理论上仅有PD-L1阳性的癌细胞才会对此免疫疗法具有正向反应的预测。此PD-L1病理评估水平与患者正向反应之间显现的不一致,挑战了使用抗PD-1/PD-L1疗法作为精准医学的目标,而近几年来针对这项临床未解的难题已有许多优秀的研究者投入与提出假说但至今仍未能有一致的结论与有效的解决方案。针对这项课题,研究人员推测目前检测PD-L1的方式可能尚未完备,以至于未能让PD-L1在病患检体中的检测水平成为理想有效的生物标志,从而帮助更多癌症患者使其能被更妥善地分类而接受抗PD-1/PD-L1免疫治疗。
对于绝大多数的膜蛋白而言,蛋白翻译后修饰,特别是糖基化,可通过影响蛋白质的结构及其与其他分子的相互作用来调节许多重要的细胞功能,包括蛋白质生物合成,定位和其他作用。PD-L1已被广为认知是一个高度糖基化的蛋白质,细胞表面PD-L1的N-连接糖基化占PD-L1多肽分子量的一半以上。研究人员因此进而推测,在某些病患组织检体中,其PD-L1蛋白外部可能被特定的糖基结构所覆盖,使其多肽抗原不能被PD-L1抗体辨识而结合,导致一些患者样品中产生不准确的PD-L1免疫组织化学结果,进而造成伪阴性误判,最终呈现与治疗结果相互矛盾的现象。根据此项推论,在临床上此类特定的病患群体,其癌细胞组织确实表达PD-L1蛋白,而此类病患本应可接受抗PD-1 / PD-L1治疗而具有正向反应,但由于检测上的假阴性结果,使得他们未能获得进行此项免疫治疗的宝贵良机。
在该研究中,研究人员研发了一个崭新的检验策略,使用糖苷内切酶分解除去细胞表面的糖基化修饰,使得PD-L1蛋白不受糖基化结构掩蔽,而易于被PD-L1抗体辨识。此一过程称为样品去糖基化。
首先研究人员使用一系列的肺癌和基底样乳腺癌细胞,通过重组糖苷酶消化处理,去除了整个N-连接的糖基化,呈现出了PD-L1的同质模式。随后在共聚焦免疫荧光显微镜以及酶联免疫吸附测定 (ELISA) 实验中,支持这样的观点,即PD-L1抗原区域上的聚糖阻碍了其与PD-L1抗体的相互作用,通过糖苷内切酶消化去除PD-L1 N-连接的糖基化,可用于增加靶蛋白的同质性,提高了PD-L1信号强度和与抗PD-L1抗体之结合亲和力,从而更准确地定量PD-L1水平。这可以提供及时的方法来减少假阴性患者分类,从而指导抗PD-1/PD-L1治疗。由于细胞表面蛋白经常在不同程度上进行N-连接糖基化,因此这种去糖基化方法可作为降低抗原异质性和消除抗体检测前结构障碍的一般方法。
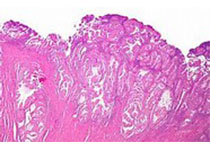
接下来,研究人员通过免疫组织化学 (IHC) 染色对来自多种器官癌组织微阵列的441个患者样本进一步探索了去糖基化,其中包括乳腺癌,肺癌,结肠癌,前列腺癌,胰腺癌和直肠癌。这些结果显示约一半的患者,其PD-L1 IHC染色水平在去糖基化后显着增加超过两倍,显示PD-L1的N-连接糖基化严重降低其对PD-L1抗体的识别。在接受免疫疗法的肺癌患者样本中,研究人员进而验证这个方法能够检测到特定的病人组织,其占整体样品数共约16%,实际上为PD-L1阳性而对于抗PD-1/PD-L1治疗呈现正向反应,但经过平行分析后此类患者若以传统检测方法却被诊断为PD-L1阴性。由于这种不准确的传统PD-L1检测方法是对患者精准分类的临床挑战,这一新研发的检测方法将提供一种实用且及时的策略,来减少用于指导抗PD-1/PD-L1治疗的假阴性患者,从而能更精确地分辨出PD-L1阳性患者,使其得以适时接受抗PD-1/PD-L1免疫疗法而获得疗效,最终将有助于临床医师精准地判断哪些癌症患者适合接受抗免疫检查点治疗而获益;此项新研发的策略可望能广泛地被应用并辅助多种癌症患者,在临床应用上有极高的价值。
总体而言,通过PD-1/PD-L1免疫检查点阻断重新激活T细胞免疫,已被证明是一种有效且很有前瞻性的癌症治疗策略。然而,PD-L1的高度糖基化阻碍了PD-L1抗体的检测,并且可能导致各种生物测定的读数不准确。除了其他已发表的疾病参数如肿瘤突变负荷和免疫细胞浸润,研究人员认为PD-L1的去糖基化优化了PD-L1的检测,使其于抗免疫检查点治疗时成为更可靠的预测性生物标志物。这项研究揭示了以糖苷内切酶去除糖基化的崭新方法,从而增强PD-L1检测而帮助筛选适当的病患接受免疫疗法。研究人员预期此研究不仅在PD-L1的临床检测上能提供直接实际的应用,其在临床科学概念上的发现也能带来革命性的突破,对于将来其他癌症标靶分子的临床检测提供了另一种可能的改进策略,藉由优化精准化医疗而造福更多免疫治疗患者。
该文章的通讯作者为洪明奇教授,前得克萨斯大学 MD 安德森癌症中心基础研究副校长,分子与细胞肿瘤学系主任,现任“台湾”中国医药大学校长。共同一作为李恒焕博士与王盈乃博士。此项研究成果是由国际团队合作而完成的,包括中国医药大学、高雄长庚纪念医院、义守大学医院、哈尔滨医科大学附属肿瘤医院以及美国德州大学安德森癌症中心。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#检出率#
0
#CEL#
28
#cancer cell#
34
#新方法#
28
#Cell#
30
#PD-L1#
24
#PD-L1阳性#
37