Cell Rep:科学家成功解析乳腺癌和卵巢癌风险相关蛋白复合体的精细结构
2017-01-16 佚名 生物谷
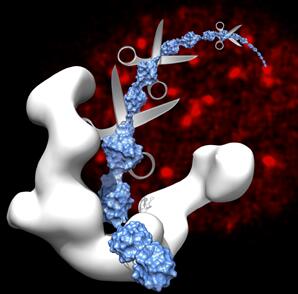
图片来源:medicalxpress.com 近日,来自英国弗朗西斯-克里克研究所(Francis Crick Institute)的研究人员通过研究描述了一种关键肿瘤抑制蛋白的分子结构,或为后期阐明该蛋白在细胞中的关键角色提供新的思路,相关研究刊登于国际杂志Cell Reports上。 BRCA1是一种人类机体基因,其能够产生名为BRCA1的肿瘤抑制蛋白,该基因突变会导致个体在一

图片来源:medicalxpress.com
近日,来自英国弗朗西斯-克里克研究所(Francis Crick Institute)的研究人员通过研究描述了一种关键肿瘤抑制蛋白的分子结构,或为后期阐明该蛋白在细胞中的关键角色提供新的思路,相关研究刊登于国际杂志Cell Reports上。
BRCA1是一种人类机体基因,其能够产生名为BRCA1的肿瘤抑制蛋白,该基因突变会导致个体在一生中出现65%-75%患乳腺癌的可能性;同时高风险乳腺癌的家族成员也都会进行BRCA1和相关的BRCA2基因的突变筛查。当然BRCA1蛋白在机体DNA修复过程中也扮演着保护性的角色,同时还能够帮助维持机体的遗传稳定性。
BRCA1基因的突变会导致相应蛋白产生不足,进而就会抑制DNA修复,从而导致机体出现遗传不稳定性的表现,而遗传不稳定就会增加个体患癌的可能性。BRCA1蛋白能够同三种蛋白复合物发生相互作用(BRCA1-A、BRCA1-B和BRCA1-C)。文章中研究者就描述了BRCA1-A蛋白的分子结构,同时深入阐明了其在细胞泛素降解过程中的关键角色,泛素降解能够参与对DNA修复机制的调节。
本文中,研究者利用一系列先进技术进行研究,比如电子显微镜检查术、质谱分析和生化分析;电子显微镜检查术能够用来解析蛋白复合物的整体形态,但其并不能针对性地检查单一份子组分的精确位点。将质谱法和生化分析法相结合就能够为科学家提供额外的信息来对组分的位点进行三角化测量。
长期以来,研究者们一直希望能够理解蛋白复合物的结构和功能,从而帮助开发BRCA1-A及相关复合物的新型抑制剂以供临床使用。研究者Steve Smerdon表示,在低分辨率下,蛋白复合物的结构仅仅是主要BRCA1复合体的结构一瞥而已;本文研究中我们所阐明的结构能够帮助我们阐明整体复合物架构如何能够稳定与泛素链的相互作用,更为重要的是,我们还阐明了如何与BRCA1相互作用才能够调节BRCA1的活性。
原始出处
Otto J.P. Kyrieleis5, Pauline B. McIntosh5, Sarah R. Webb, Lesley J. Calder, Janette Lloyd, Nisha A. Patel, Stephen R. Martin, Carol V. Robinson, Peter B. Rosenthal, Stephen J. Smerdon.Three-Dimensional Architecture of the Human BRCA1-A Histone Deubiquitinase Core Complex.Cell Rep.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#乳腺癌和卵巢癌#
39
#CEL#
38
#解析#
37
#复合体#
29
#癌风险#
28
#Cell#
29