CELL RES:癌症免疫治疗及精准医学进展
2017-01-17 MedSci MedSci原创
利用免疫系统来根除肿瘤细胞正在成为一种最有力的新型癌症治疗方法。那么目前关于这一热点话题的研究进展如何呢?近期一项发表在CELL RES杂志上的文章综述了癌症免疫治疗的最新进展以及新的战略在鉴定新的免疫靶点和突变衍生抗原(新抗原)对癌症免疫治疗和免疫精准医学的进展。FDA批准基于免疫治疗的药物sipuleucel-T(Provenge)、ipilimumab(抗CTLA-4)以及最近研究火热的程序
利用免疫系统来根除肿瘤细胞正在成为一种最有力的新型癌症治疗方法。那么目前关于这一热点话题的研究进展如何呢?
近期一项发表在CELL RES杂志上的文章综述了癌症免疫治疗的最新进展以及新的战略在鉴定新的免疫靶点和突变衍生抗原(新抗原)对癌症免疫治疗和免疫精准医学的进展。
FDA批准基于免疫治疗的药物sipuleucel-T(Provenge)、ipilimumab(抗CTLA-4)以及最近研究火热的程序性细胞死亡抗体-1(PD-1)(pembrolizumab,派姆单抗)在治疗多种类型的癌症中显示出了在癌症免疫治疗领域和临床研究中的显著进展。
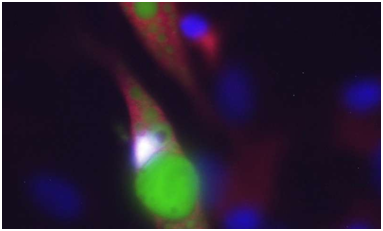
此外,使用NY-ESO-1特异性T细胞受体(TCR)或CD19嵌合抗原受体(CAR)的一些近期临床试验已经对转移性癌症患者显示出了很有希望的临床结果。
目前癌症免疫治疗的成功是基于20年前鉴定的癌抗原和共抑制信号分子的工作之上的。在大量的靶抗原中,CD19是用于治疗血癌的CAR T细胞的最佳靶点,但是CAR-工程化T细胞免疫治疗在实体癌中尚未起作用。NY-ESO-1是实体癌中基于TCR的免疫治疗的最佳靶标之一。尽管检查点阻断治疗取得了巨大成功,但是仍有超过50%的癌症患者不能对阻断治疗作出反应。
新技术(如下一代测序)的出现增强了我们在肿瘤免疫学中寻找新的免疫靶标的能力,并加速了可能更广泛地覆盖癌症患者的免疫治疗的发展。
原始出处:
Wang RF, Wang HY. Immune targets and neoantigens for cancer immunotherapy and precision medicine. Cell Res. 2017 Jan;27(1):11-37. doi: 10.1038/cr.2016.155.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
33
#医学进展#
47
很好,不错,以后会多学习
72
#Cell#
34
#精准#
36