Ther Adv Med Oncol:转移性结直肠癌治疗新进展
2017-08-21 月下荷花 肿瘤资讯
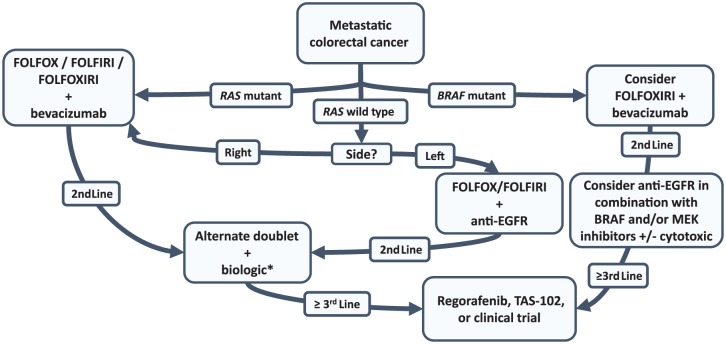
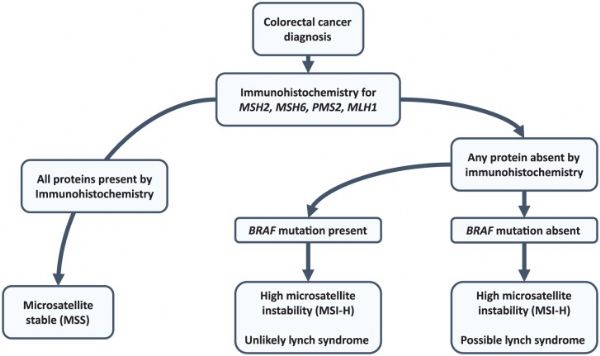
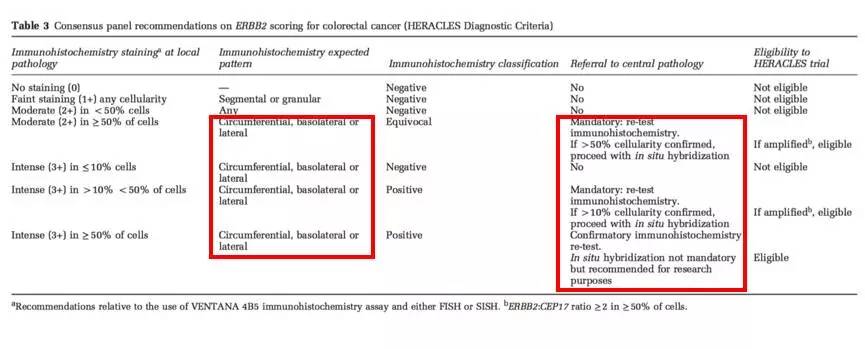
过去10年里几乎没有mCRC新作用机制药物问世,但CRC分子机制有大量进展,组织测序和液体活检可鉴定CRC分子特征指导治疗,改善对肿瘤异质性和遗传学进化的认识。美国Loree教授在Ther Adv Med Oncol上发文细述了对临床实践有改变的药物进展, 讨论了分子亚型和生物标志的重要性,以及治疗流程可能发生的改变。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了多谢分享
62
学习了谢谢分享
56
#转移性#
42
#结直肠#
38
#Med#
35
#Oncol#
23
非常好的文章,学习了,很受益
62