JCO:PARP抑制剂veliparib进军广泛期小细胞肺癌一线,小细胞肺癌又多了一种治疗方式?
2019-01-07 肿瘤资讯编辑部 肿瘤资讯
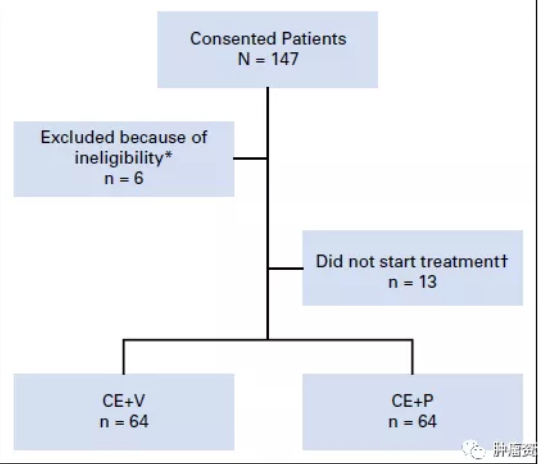
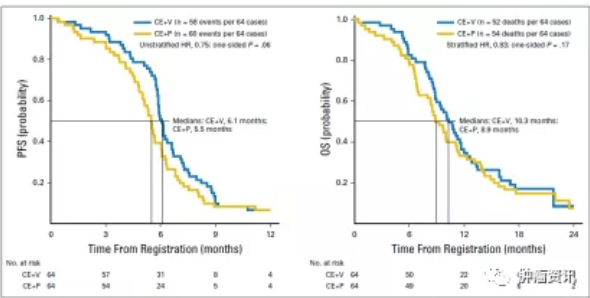
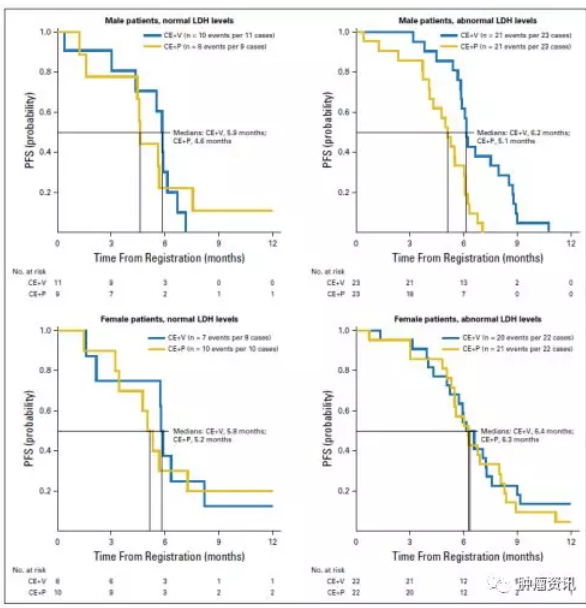
Veliparib是一种多聚(ADP核糖)聚合酶PARP抑制剂。临床前研究结果显示, veliparib或可增强小细胞肺癌标准化疗的疗效。ECOG-ACRIN 2511研究是一项随机II期研究,探究了veliparib联合顺铂和依托泊苷一线治疗是广泛期小细胞肺癌(ES-SCLC)患者的疗效。近期,该项研究的结果荣登Journal of Clinical Oncology杂志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCO#
35
#抑制剂#
33
#治疗方式#
44
#广泛期小细胞肺癌#
27
#Veliparib#
36
#PARP#
36