Neurosurgery:『首过效应』诊断颅内动脉粥样硬化性闭塞的意义
2019-08-08 杨中华 脑血管病及重症文献导读
亚洲人中颅内动脉粥样硬化很常见,占缺血性卒中的25%-50%。在亚洲,颅内动脉粥样硬化(intracranial atherosclerotic stenosis,ICAS)急性闭塞的发生率大约为22.9%;在西方国家为5.5%。
亚洲人中颅内动脉粥样硬化很常见,占缺血性卒中的25%-50%。在亚洲,颅内动脉粥样硬化(intracranial atherosclerotic stenosis,ICAS)急性闭塞的发生率大约为22.9%;在西方国家为5.5%。机械取栓是治疗颅内闭塞性急性缺血性卒中的有效治疗方法,但是该方法主要为栓塞性闭塞设计的,而不是 ICAS。机械取栓再灌注后再闭塞常常发生于 ICAS 的部位,与血小板聚集有关。这样,挽救性治疗比如紧急血管成形术或支架,是必要的。因此,鉴别 ICAS 和颅内栓塞是非常重要的。
高分辨血管壁 MRI 可以检测和评价 ICAS。然而,这些检查往往需要3.0T 或7.0T 的 MR 扫描仪,大部分医院不具备这个条件。另外,MR 检查耗时,并且需要患者配合。血管内治疗期间鉴别 ICAS 和颅内栓塞是一种实用和省时的解决办法。
在临床实践中,福建医科大学漳州附属医院的Ting-Yu Yi等发现了一种现象称为微导管『首过效应』(first-pass effect),特别常见于 ICAS 患者。首过效应是指在血管造影过程中,当微导管向前通过闭塞的部位,然后把微导管收回到闭塞部位的近端时可以看到闭塞部位血管管腔内有缓慢和暂时的血流,这个现象他们称为首过效应。
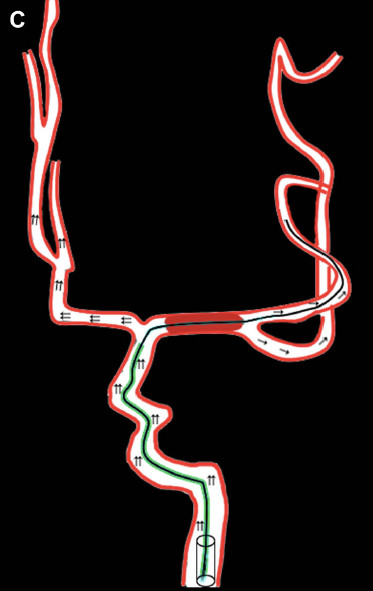
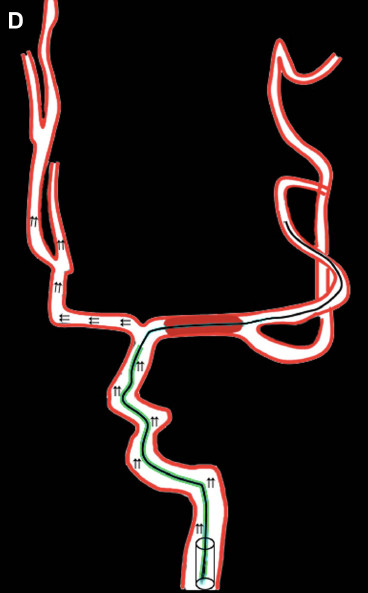
示意图:微导管首次通过效应。A 图,左侧 MCA 闭塞。B 图,在微导丝的指引下微导管通过血栓:
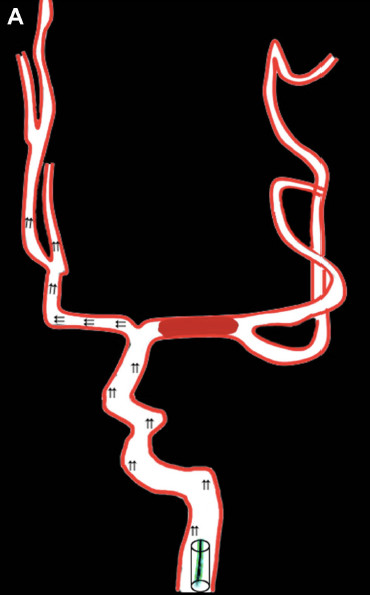
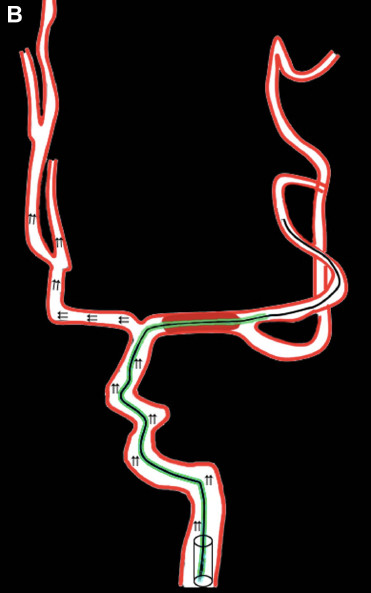
C 和 D 图,微导丝保持原位,收回微导管。C 图,血栓远端可见到缓慢的血流,称为首次通过效应。D 图,血栓远端无血流,提示不存在首次通过效应:
2019年6月Ting-Yu Yi等在NEUROSURGERY上公布了他们的回顾性研究结果,目的在于评价首过效应能否鉴别 ICAS 和颅内栓塞。
该研究共纳入了61例颅内大动脉闭塞性急性缺血性卒中患者。他们发现首次通过效应更常见于 ICAS(ICAS 和颅内栓塞:90.9% vs 12.8%,P<0.001)。微导管首次通过效应识别ICAS 的敏感性、特异性、阳性预测值和精确性分别为90.9%, 87.2%, 80.0%, 88.5%。
最终作者认为微导管首次通过效应预测急性症状性 ICAS 的敏感性和阳性预测值都很高。
译者注:对于急性缺血性卒中血管内治疗来讲,识别是否为 ICAS 具有非常重要的意义。以下情况可能提示 ICAS 颅内大动脉闭塞1.病史;2.常见的影像学证据,比如SWI磁敏感血管征阴性,Flair 血管高信号征,CT 大脑中动脉高密度征往往提示心源性;3.取栓过程中的证据,比如微导管首次通过效应,取栓后残留狭窄,需要支架植入,取出血栓的性状(比如颜色越深越提示富含红细胞,更提示心脏来源,反之亦然)。
原始出处:Yi TY1, Chen WH1, Wu YM1, et al. Microcatheter "First-Pass Effect" Predicts Acute Intracranial Artery Atherosclerotic Disease-Related Occlusion. Neurosurgery. 2019 Jun 1;
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#surgery#
48
#粥样硬化#
52
#粥样硬化性#
47
#GER#
35
#颅内动脉粥样硬化#
45
#ROS#
37
#硬化性#
33