Nat Commun:肿瘤细胞代谢重编程与周期调控新机制
2017-11-17 佚名 中国科学技术大学
中国科学技术大学生命学院张华凤课题组、高平课题组联合中科院合肥物质科学研究院强磁场科学中心王俊峰课题组,在肿瘤细胞的代谢重编程与周期调控研究领域取得进展,相关研究成果以Polo-like Kinase 1 Coordinates Biosynthesis during Cell Cycle Progression by Directly Activating Pentose Phosphate P
中国科学技术大学生命学院张华凤课题组、高平课题组联合中科院合肥物质科学研究院强磁场科学中心王俊峰课题组,在肿瘤细胞的代谢重编程与周期调控研究领域取得进展,相关研究成果以Polo-like Kinase 1 Coordinates Biosynthesis during Cell Cycle Progression by Directly Activating Pentose Phosphate Pathway为题,15日在线发表在Nature Communications上。
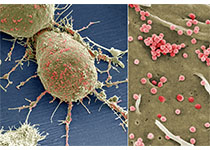
肿瘤代谢重编程和细胞周期调控异常是肿瘤的两个重要特征,然而人们尚不清楚这两者之间如何相互协调以促进肿瘤细胞的增殖和肿瘤的发生发展。课题组首次发现在肿瘤细胞中,重要的周期调控蛋白Plk1在周期进程中调节磷酸戊糖途径的关键代谢酶G6PD的活性,并进而促进生物大分子合成以及肿瘤细胞在体内外的增殖。进一步的机制研究发现,Plk1通过结合并磷酸化修饰G6PD,使G6PD形成二聚体增多,从而促进酶活性以及整个磷酸戊糖途径。增强的磷酸戊糖途径对于肿瘤细胞的周期进程以及肿瘤的发生发展有重要的促进作用。该研究首次发现了周期调控蛋白Plk1在调节生物大分子合成方面的新功能,揭示了代谢重编程与周期调控相互协调共同促进肿瘤细胞快速增殖的新机制,对临床肿瘤的靶向治疗有潜在的指导意义。
研究工作在国家自然科学基金委、科技部以及中科院的资助下完成。
原始出处:
Xiaoyu Ma,et al.,Polo-like kinase 1 coordinates biosynthesis during cell cycle progression by directly activating pentose phosphate pathway.Nat Commun.15 November 2017.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#COMMUN#
29
#肿瘤细胞代谢#
35
#Nat#
31
#肿瘤细胞#
32
#细胞代谢#
36