JAMA Intern Med:结肠镜筛查**二氧化碳气腹
2016-06-22 Mechront 译 MedSci原创
“虽然许多美国人经常接受结肠镜筛查,但没有随机试验量化筛选对结直肠癌的发病率和死亡率的影响,”挪威奥斯陆大学经济系健康管理的Michael Bretthauer博士说,“当前发表在JAMA Internal Medicine的NordICC试验,是目前已知的对结肠镜筛查的首次评价,比较了筛查或不筛查对结直肠癌发病率和死亡率的影响。”虽然结直肠癌是高收入国家的第二大癌症,但大多数欧洲国家并没有引入结
“虽然许多美国人经常接受结肠镜筛查,但没有随机试验量化筛选对结直肠癌的发病率和死亡率的影响,”挪威奥斯陆大学经济系健康管理的Michael Bretthauer博士说,“当前发表在JAMA Internal Medicine的NordICC试验,是目前已知的对结肠镜筛查的首次评价,比较了筛查或不筛查对结直肠癌发病率和死亡率的影响。”
虽然结直肠癌是高收入国家的第二大癌症,但大多数欧洲国家并没有引入结肠镜检查的筛查。为了更好的了解这些国家,Bretthauer和同事在挪威,瑞典,波兰和荷兰进行了一项基于人群的结肠镜筛查的随机试验。该试验包括94959名年龄在55至64岁的结直肠癌平均风险的人。研究人员调查了结肠镜筛查的参与率、腺瘤的产量、性能和不良事件。
总体而言,结肠镜筛查的参与率为40%,挪威的参与率为60.7%,瑞典为22.9%,波兰为33%,荷兰为39.8%(P < .001)。盲肠插管率为97.2%,有77.4%没有接受镇静。那些接受结肠镜筛查的参与者中,有一个穿孔(0.01%)、两个息肉浆膜烧伤(0.02%)、18例息肉出血(0.14%)。
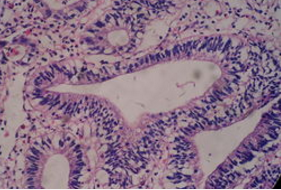
在同一组中,62名受试者(0.5%)被诊断为结直肠癌。此外,有30.7%的参与者有腺瘤,其中10.4%被认为是高风险。盲肠插管推荐率(95%)和腺瘤的检出率(25%)与内镜师不符合(17.1%和28.6%),表明不同内镜医师的性能显著不同。此外,标准空气注入技术和co2气腹相比,中度至重度腹痛的患者分别有16.7%和4.2% (P < .001)。
研究者说,“国家和个人之间内镜医师的显著差异还值得进一步的研究,此外结肠镜检查中标准空气注入技术应该放弃,而青睐于co2气腹。”
原始出处:
Bretthauer M, et al. Population-Based Colonoscopy Screening for Colorectal Cancer.JAMA Intern Med. 2016;doi:10.1001/jamainternmed.2016.0960.
Carbon dioxide insufflation preferred over air insufflation in colonoscopy screening.Healio.June 21, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












不错哦,会学到很多
81
#气腹#
40
#肠镜#
38
#二氧化碳#
35
#Med#
32