Injury:三束缝合法治疗急性跟腱断裂手术技术
2014-07-16 童勇骏 丁香园
急性跟腱断裂最佳治疗方案在临床上存在较多争议。有研究发现,急性跟腱锻炼通过保守石膏制动固定或者手术修复等均可以取得愈合,并且功能基本类似;两者的差别在于,前者有更高的再断裂率,后者有更高的并发症发生率。 中国的临床医生通常主张对跟腱断裂采取更为激进的手术治疗,手术缝合断端跟腱时较为常用的是Krakow锁边缝合法(Krakow locking loop technique,图1);Jaakkola
急性跟腱断裂最佳治疗方案在临床上存在较多争议。有研究发现,急性跟腱锻炼通过保守石膏制动固定或者手术修复等均可以取得愈合,并且功能基本类似;两者的差别在于,前者有更高的再断裂率,后者有更高的并发症发生率。
中国的临床医生通常主张对跟腱断裂采取更为激进的手术治疗,手术缝合断端跟腱时较为常用的是Krakow锁边缝合法(Krakow locking loop technique,图1);Jaakkola等人则在2000年时提出一种三束缝合法(triple bundle technique,图2)进行跟腱修复,并且通过尸体学研究证明,该缝合法的跟腱力学强度和术后并发症要好于krakow锁边缝合法。

图1:Krakow锁边缝合法

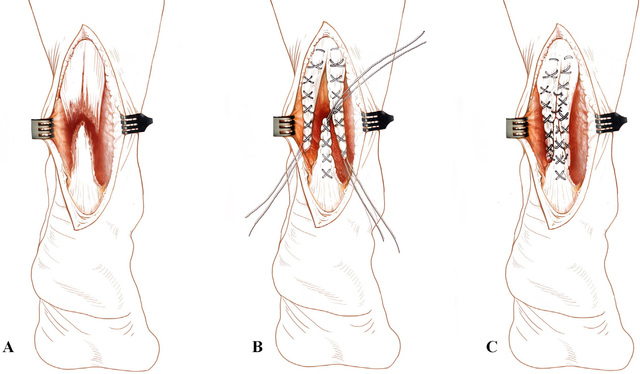
图2:跟腱断裂三束缝合法,其最基本的思路是,通过对断端跟腱的修整,将不平整的断端跟腱重建为类似肌腱断端的三个头,而后通过肌腱缝合技术,将每个断端缝合。手术技术:患者俯卧位,大腿部位捆扎止血带,取后内侧纵行切口,全层切开至肌腱旁组织,仔细分离周围组织,暴露断端跟腱,清创,冲洗,清除断端血肿等,注意,此时前往不要损伤跟腱前侧的血供,A;将剩余的跟腱断端组织整理成三束,近端两束,远端一束,使用2号可吸收缝合线,采用Bunnell缝合技术缝合三束跟腱,B;完成上述步骤后,将近端两束和远端一束分别按照端端缝合法进行缝合修复,注意,修复时仅保持断端适当的张力,勿过度缩短跟腱,C。
近日,有意大利学者对三束缝合法治疗跟腱断裂的长期功能预后进行随访报道,发现,该手术方法可提供较好的力学强度,以方便患者进行早期功能锻炼;术后的并发症更少。
研究者对66例单侧跟腱完全断裂的患者使用了三束缝合法进行跟腱修复手术。术后比较患肢和健肢的AOFAS(American Orthopaedic Foot and Ankle Society)评分,Leppilahti评分,踝关节运动度,大腿、腓肠肌、踝关节周径,踝关节动力学参数等指标,以确定术后患者跟腱功能恢复情况。
术后发现,约80%的患者可以恢复术前的运动水平,术后3年,AOFAS评分及Leppilahti评分分别为93.9,91.8。仅2例患者出现腓肠肌肌肉萎缩,1例患者出现疤痕愈合。无患者出现跟腱再断裂。术后3年随访时,踝关节屈伸功能良好。
作者认为,该手术技术可以提供较好的修复效果,术后并发症少,应该成为跟腱断裂修复时的一个备选术式。
原始出处
Bevoni R1, Angelini A2, D'Apote G3, Berti L3, Fusaro I4, Ellis S5, Schuh R6, Girolami M1.Long term results of acute Achilles repair with triple-bundle technique and early rehabilitation protocol.Injury. 2014 Aug;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#手术技术#
42
#跟腱断裂#
38
#急性跟腱断裂#
51
#Injury#
40