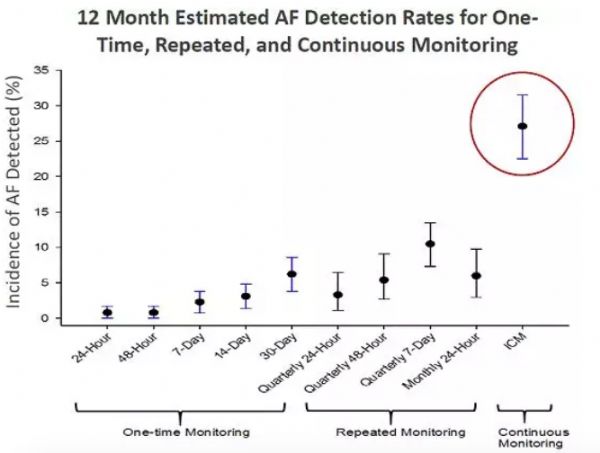
Circ:Cardiovasc Inte:经皮左心耳封闭术是脑血管病高危房颤患者的合理选择
2018-03-18 xiangting MedSci原创
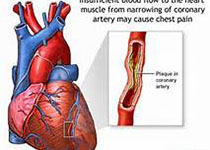
LAA封闭主要用于合并症多且预后差的患者。这类患者进行LAA封闭似乎可以合理降低卒中发生率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
26
#血管病#
25
#左心耳#
32
#房颤患者#
28
不错耶.学习了
54