本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

荷兰一项研究表明,儿童期房间隔缺损(ASD)手术闭合的极远期转归较佳,伴有良好生存率和较低发病率。论文于7月25日在线发表于《心脏》(Heart)。 此项纵向队列研究共纳入135例于年龄<15岁时接受ASD手术修补的序贯性患者。患者接受心电图、心脏超声、运动试验、N端脑利钠肽前体测定、Holter监测和心脏MRI扫描等检查。主要转归指标为生存率、心室功能以及心脏再介入、卒中、症状性心律失常
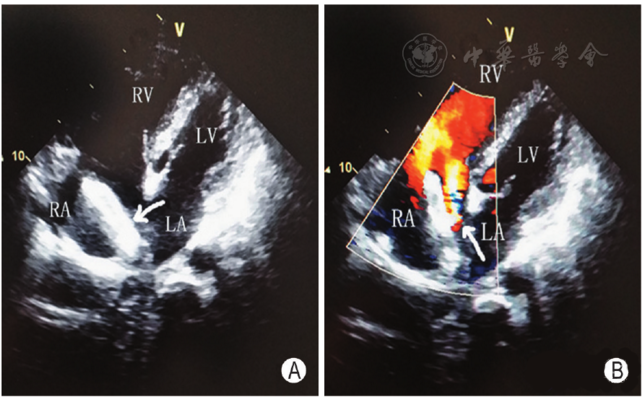
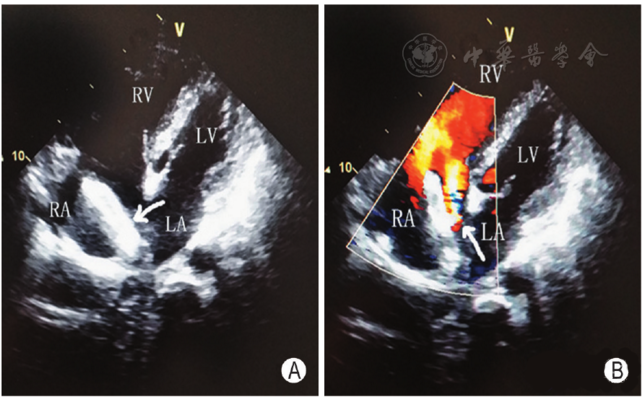
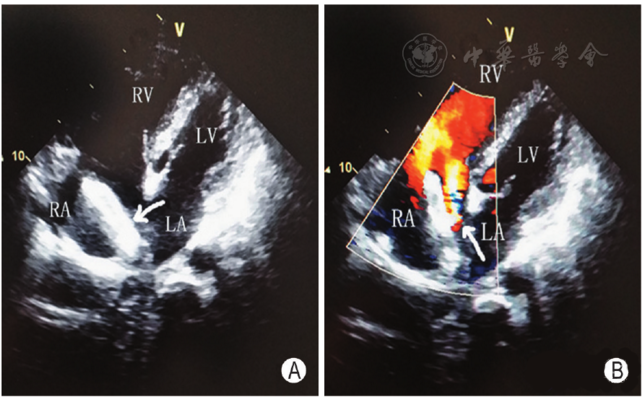
西安交大一附院心血管病医院张玉顺教授团队近日成功完成一例心房颤动合并房间隔缺损患者的左心耳与房间隔缺损联合封堵手术。目前患者已康复出院。该患者有多年房颤病史,同时合并高龄女性、高血压病、短暂性脑缺血发作、肝功能异常等多重危险因素,近期病情加重,危及生命。在充分权衡患者血栓栓塞风险与服用抗凝药物的出血风险后,张玉顺教授与患者及家属充分交流后决定实施左心耳封堵手术,降低栓塞风险的同时也避免出血风险增加
新发偏头痛是房间隔缺损(ASD)封堵术(经导管)后常见的并发症之一,有研究表明氯吡格雷可加上良好ASD封堵术后的偏头痛发生。研究者进行了一项试验,评估氯吡格雷+阿司匹林对ASD封堵术后偏头痛发生率的影响。该随机、双盲研究共纳入171名无偏头痛病史的ASD患者,按1:1分为氯吡格雷+阿司匹林组(n=84)和单独阿司匹林+安慰剂组(n=87)。在ASD封堵术后治疗3个月。治疗期间每月偏头痛天数为初始指
房间隔缺损(ASD)为临床上常见的先天性心脏畸形,常伴发出现心房纤颤、心房扑动等心律失常,带来血栓形成和卒中发作等严重并发症,研究指出房缺行修补治疗后房颤发生风险增高。为评估房间隔缺损(ASD)患者的房颤和卒中风险较普通人群是否有明显差异,以及房缺行修复后房颤和卒中风险变化情况,丹麦的一些研究者展开了这项对照研究,近日将研究发表在Heart杂志上 从1977年到2009年,研究者收集了丹麦境内被诊
加拿大学者的一项研究表明,在法洛四联症(ToF)和房间隔缺损(ASD)患者中,慢性容量负荷对右室整体和局部心肌变形影响各异,提示这两种疾病具有不同的适应性机制,也表明应变测量受心室体积的影响,在解释应变值时应予以考虑。论文于2012年11月2日在线发表于《国际心脏病学杂志》(Intern J Cardiol)。
经导管ASD封堵术后的长期随访期间TR显著降低。重度/中度TR患者的心衰症状有所改善。


梅斯医学MedSci APP
医路相伴,成就大医
#心动图#
17
#房间隔缺损#
34
非常好的文章.学习了
57
学习
0
学习了.谢谢分享!
64
学习了.谢谢.
67