FDA批准强生前列腺癌新疗法 可延长生存期超2年
2018-02-25 孙欢/编译 健康时报网
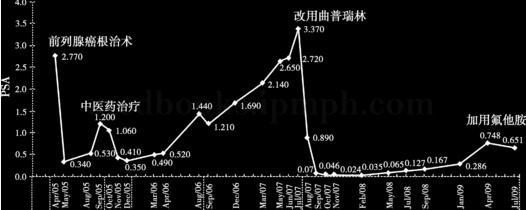
近日,美国食品药品监督管理局(FDA)宣布,批准强生(Johnson & Johnson)旗下的杨森(Janssen)公司下一代雄激素受体抑制剂Erleada(apalutamide),用于治疗非转移性去势抵抗性前列腺癌(NM-CRPC)患者。这些患者虽然在接受激素治疗,但肿瘤仍继续增长。值得一提的是,它是首个经FDA批准的用于非转移性去势抵抗性前列腺癌的疗法。美国国立卫生研究院的国家癌
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#FDA批准#
31
#强生#
34
#生存期#
28
#新疗法#
30
一起学习学习
50
学习了.涨知识
53
阅
50
很好
54