GW-ICC2017:张静:重症心力衰竭的有创血流动力学监测
2017-10-18 佚名 国际循环
血流动力学监测能是重症心力衰竭(心衰)治疗过程中必不可少的组成部分,合理的血流动力学监测方法指导治疗决策能事半功倍。在GW-ICC 2017上,河南省人民医院的张静教授就重症心衰患者的有创血流动力学监测作了专题讲座,详细介绍了各种有创血流动力学监测方法对于重症心衰患者的意义。
血流动力学监测能是重症心力衰竭(心衰)治疗过程中必不可少的组成部分,合理的血流动力学监测方法指导治疗决策能事半功倍。在GW-ICC 2017上,河南省人民医院的张静教授就重症心衰患者的有创血流动力学监测作了专题讲座,详细介绍了各种有创血流动力学监测方法对于重症心衰患者的意义。
重症心衰简介
重症心衰包括急性心衰、难治性心衰、心源性休克及心衰合并其他脏器功能损害(如肝脏及肾脏损害等)。其中,急性心衰是指心衰的症状及体征突然发作或短期内恶化加重,需要紧急住院治疗、危及生命的紧急情况;难治性心衰定义为反复住院或需要长期静脉血管活性药物或其他方法维持的情况。
血流动力学监测概述
血流动力学监测是指根据物理学定律、结合生理和病例生理学概念,对循环系统中血液运动的规律性进行定量、动态、连续测量和分析,以了解病情发展并指导临床治疗。其有助于鉴别血流动力学异常的病因、监测氧合情况及观察对治疗的反应,分为无创性血流动力学监测和有创性血流动力学监测两大类。其中,前者包括心电图、无创血压、脉搏血样饱和度、无创心排量等,后者包括有创动脉血压、中心静脉压(CVP)、肺动脉压、有创心排出量(CO)和脉搏指示持续心输出量(PICCO)等。
重症心衰的血流动力学监测方法优劣势分析
有创动脉血压监测
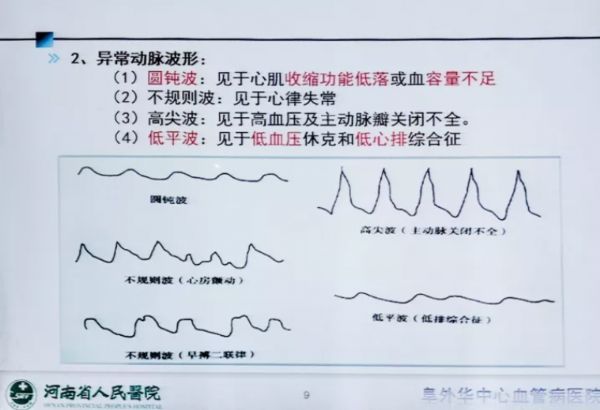
有创动脉血压监测是经动脉穿刺置管后直接测量血压的方法,能反映每个心动周期的血压变化情况。其优点在于对血管痉挛、休克、体外循环的患者测压结果更可靠,缺点在于可导致血肿、血栓及感染等。就重症心衰患者,选择有创血压监测的数据更准确、详细,可提供即时、持续和直观的血压变化。此外,通过观察压力波形,临床医生可间接估计血容量、心肌收缩力、心排血量等,并在心电图受干扰时提供心率及心律的变化(图1)。
图1. 有创动脉血压监测常见异常波形及其临床意义
CVP监测
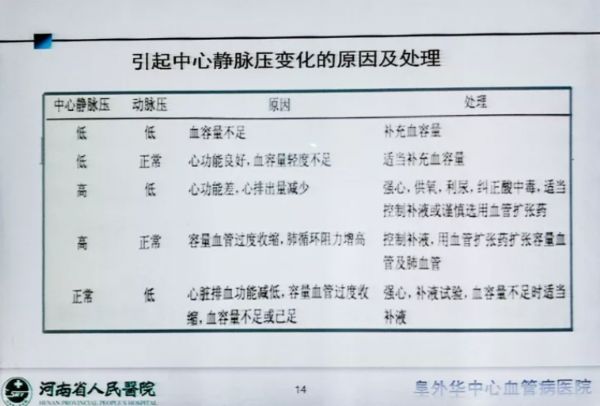
CVP是对右心室充盈压的直接测量,其正常范围为5~12 cm H2O。CVP可为评价患者容量状态、有无心包填塞、右心功能、心脏顺应性等提供线索,有助于提供适当的充盈压以保证心排出量,此外,因心排出量不能常规测量,临床工作中常依据动脉压结合CVP变化等对病情作出判断并指导治疗(图2)。
图2. 引起CVP变化的原因及其处理
肺动脉压及肺毛细血管楔压监测
临床实践中,因CVP无法反映左心功能,患者存在左心功能不全时有必要进行肺动脉压(PAP)和肺毛细血管楔压(PAWP)监测。PAP所示的收缩压、舒张末压及平均压正常值分别为15~25 mm Hg、8~15 mm Hg和10~20 mm Hg。其代表右心室收缩产生的收缩期压力,反映肺小动脉和肺毛细血管床的流量或梗阻情况。PAP增高提示肺脏疾病、肺血管阻力增高、二尖瓣狭窄或反流、左心衰、血流增多或存在左向右分流;降低则提示低血容量、肺动脉瓣狭窄及三尖瓣狭窄。
PAWP正常值为6~12 mm Hg,反映肺部循环状态,是判断肺充血及其程度的指标,与左心房平均压密切相关。因此,PAWP降低提示低血容量或换能器零点过高;增高则提示液体负荷过重、左心衰、二尖瓣狭窄或反流及心肌梗死等。
CO
CO是指一侧心室每分钟射出的总血量,正常值为5.0~6.0 L/min,是反映心泵功能的重要指标,其对评价患者心功能具有重要意义,对于补液、输血和心血管药物治疗有指导意义。此外,还可通过CO计算其他血流动力学参数(如心脏指数)。
PICCO
PICCO即脉搏指示持续心排出量监测,是经肺热稀释法和动脉脉搏轮廓分析法来综合对血流动力学和容量进行监护管理,可评估心脏前负荷、心脏后负荷、心肌收缩力等。其可测量全心相关参数及全心舒张末期容积、胸腔内血液容积,更充分地反映心脏前负荷变化。
综上所述,每一种监测方法均有其各自的优点和缺点,任何监测方法都不应脱离疾病的临床表现。因此,临床医生应将上述指标与临床表现相结合,旨在对重症心衰作出及时准确的诊治。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#血流动力#
21
#血流动力学#
29
#ICC#
0
#GW-ICC#
33