Sci Transl Med:癌细胞“大义灭亲”!哈佛科学家将癌细胞改造成冷血抗癌杀手,杀遍全身肿瘤后自杀
2018-07-30 奇点糕 奇点网
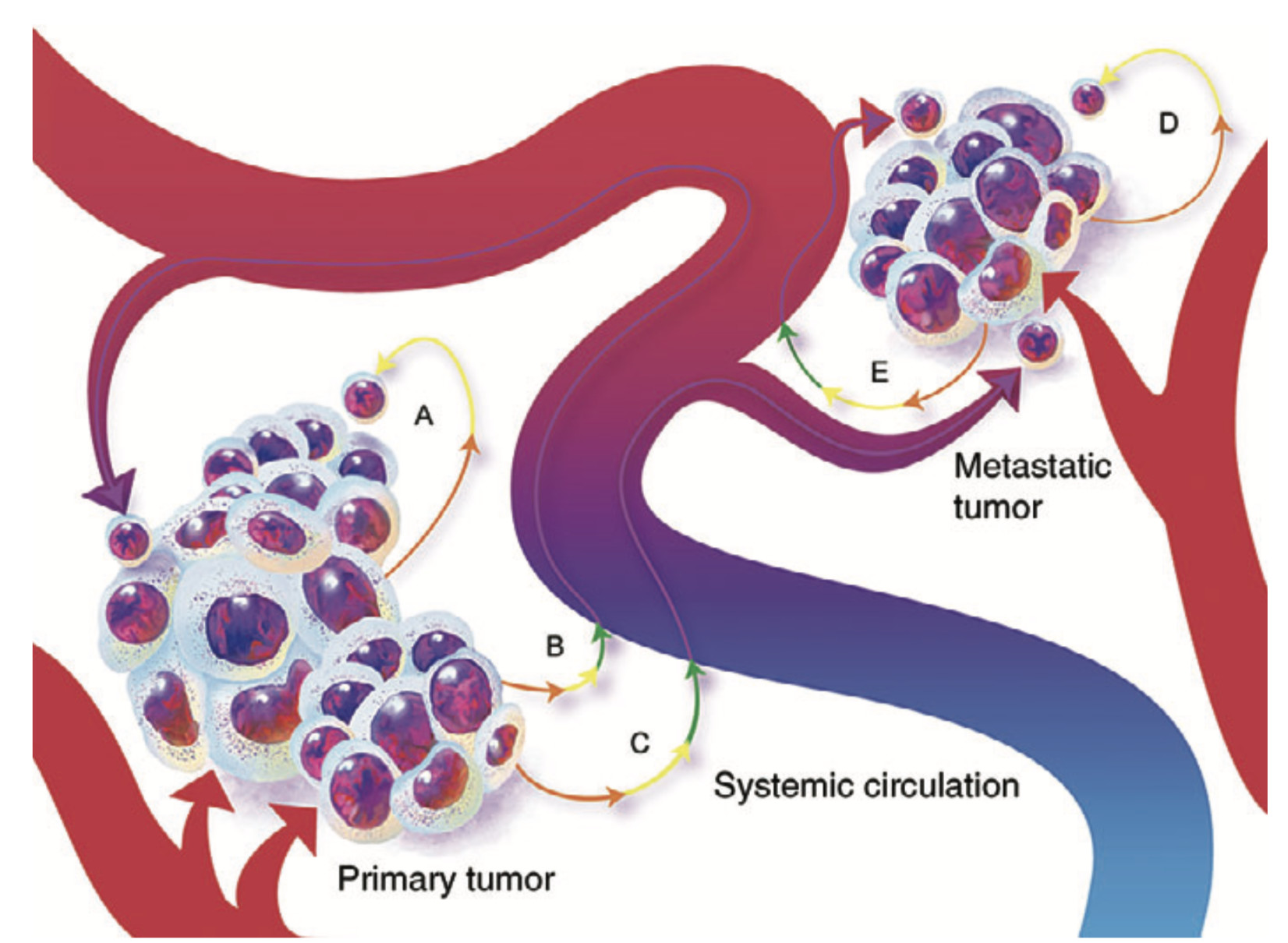
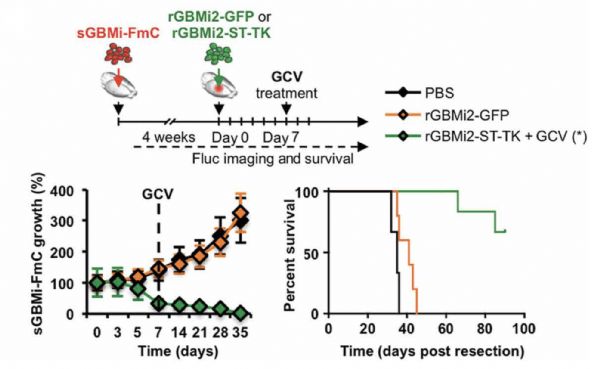
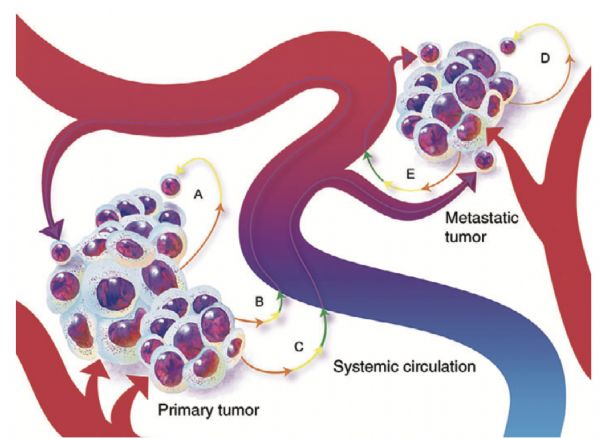
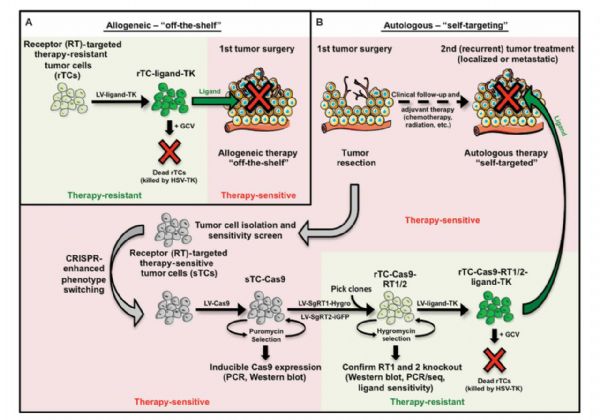
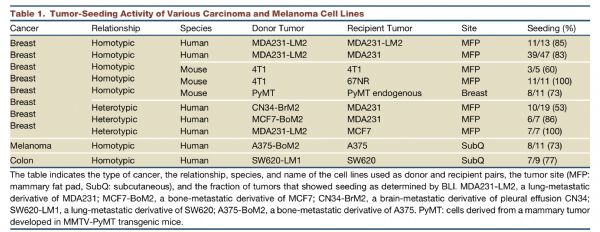
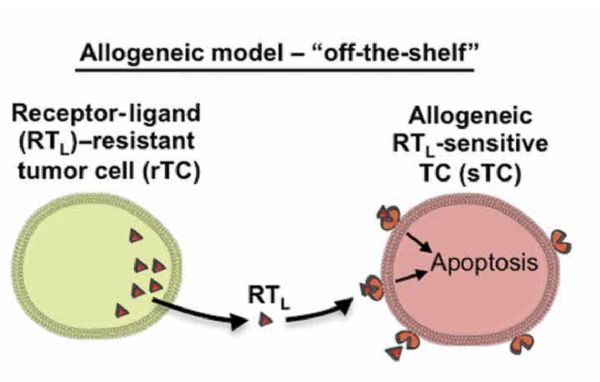
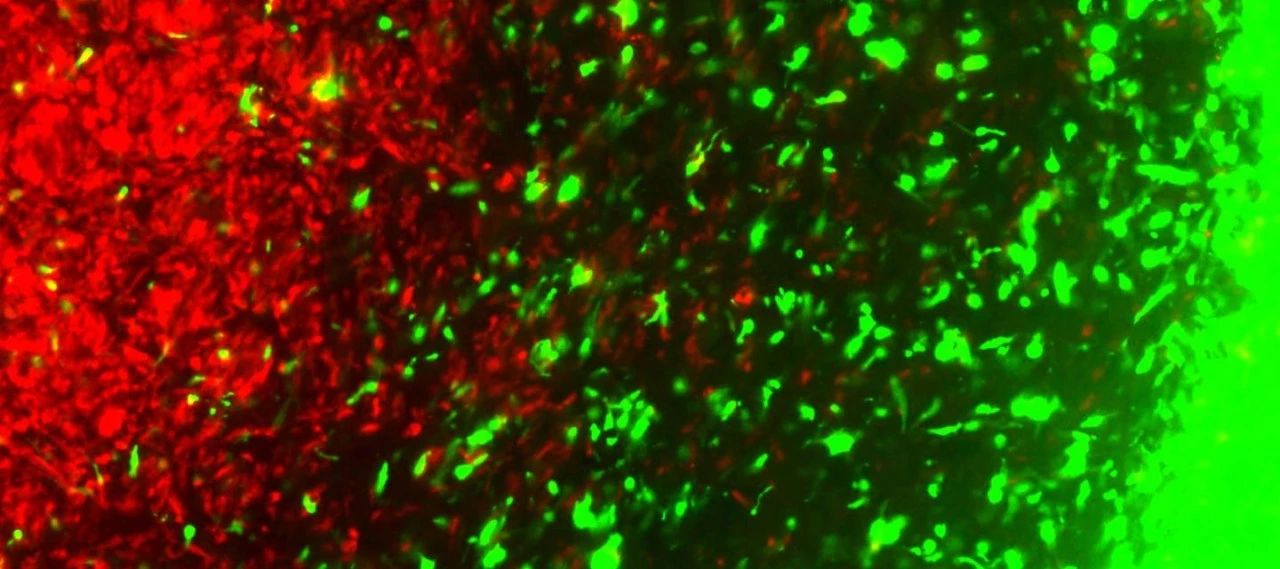
近日,哈佛医学院附属医院——布列根和妇女医院——的Khalid Shah研究团队,给恶性肿瘤回敬了一个大礼。他们用CRISPR基因编辑技术,把癌细胞改造成抗癌杀手,利用癌细胞的“归巢”特点,直捣黄龙。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Transl#
41
#TRA#
34
#癌细胞#
33
#哈佛#
45
#Med#
47
学习了谢谢
68
“效果有些惨烈”,是有多大的副作用呢。
77
很创新
82
外国人怎么能研究,我们国内的天天吃别人剩饭
79
盼望通过临床,取得医学突破!
64