mSphere:研究发现谷胱甘肽在铜绿假单胞菌的毒力中发挥关键作用
2018-05-16 MedSci MedSci原创
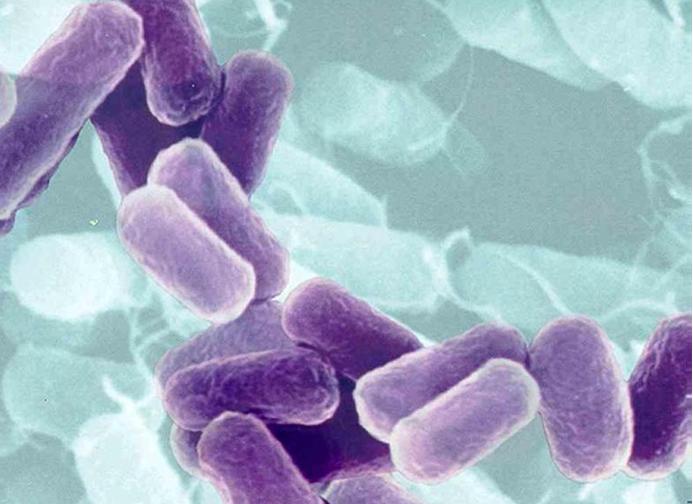
铜绿假单胞菌是一种无处不在的革兰氏阴性细菌,可导致严重的机会性感染。该菌使用的主要氧化还原缓冲液是谷胱甘肽(GSH)。为了评估GSH在铜绿假单胞菌毒力中的作用,使用缺少gshA的突变菌株进行了许多分析,该菌株不产生GSH。 结果显示,与野生型菌株相比,突变菌株在基本培养基中表现出生长延迟。此外,gshA突变体在生物膜和残留细胞形成以及游动和群集运动性方面存在缺陷,并关键毒力因子绿脓素的水平降低。最
铜绿假单胞菌是一种无处不在的革兰氏阴性细菌,可导致严重的机会性感染。该菌使用的主要氧化还原缓冲液是谷胱甘肽(GSH)。为了评估GSH在铜绿假单胞菌毒力中的作用,使用缺少gshA的突变菌株进行了许多分析,该菌株不产生GSH。
结果显示,与野生型菌株相比,突变菌株在基本培养基中表现出生长延迟。此外,gshA突变体在生物膜和残留细胞形成以及游动和群集运动性方面存在缺陷,并关键毒力因子绿脓素的水平降低。最后,gshA突变株表明对甲基紫精(氧化还原循环剂)以及巯基反应性抗生素磷霉素和利福平的敏感性增加。
总之,这些数据表明GSH在铜绿假单胞菌毒力中发挥关键作用。
原始出处:
Tricia A. Van Laar, Saika Esani, et al., Pseudomonas aeruginosa gshA Mutant Is Defective in Biofilm Formation, Swarming, and Pyocyanin Production. mSphere. 2018 Mar-Apr; 3(2): e00155-18. doi: 10.1128/mSphere.00155-18
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究发现#
25
学习了谢谢分享!
64
很好的学习机会
60
学习了
70
学习了.涨知识了!
64