Sci Tran Med:科学家发现治疗乳腺癌失败的又一大因素
2018-03-15 白木清水 来宝网
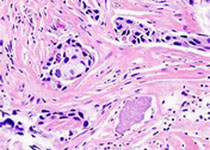
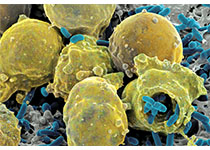
肥胖--已知会降低几种癌症的存活率,可能解释了血管生成抑制剂在治疗乳腺癌方面的无效性。一个研究小组首次发现,肥胖和肥胖相关的分子因素似乎在乳腺癌患者和两种小鼠模型中诱导了对抗血管生成治疗的抗性。 他们在“科学转化医学”中的报告还详细介绍了与这种耐药相关的特定肥胖相关因素,并概述了可能会克服它的潜在治疗策略。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TRA#
33
#科学家发现#
32
#Med#
23
不错的文章值得推荐
54
肥胖--已知会降低几种癌症的存活率.可能解释了血管生成抑制剂在治疗乳腺癌方面的无效性.一个研究小组首次发现.肥胖和肥胖相关的分子因素似乎在乳腺癌患者和两种小鼠模型中诱导了对抗血管生成治疗的抗性.
54
不错的文章值得拥有
65