ACC 2018:美国心房颤动筛查的费-效比研究
2018-03-14 高秀芳 中国医学论坛报今日循环
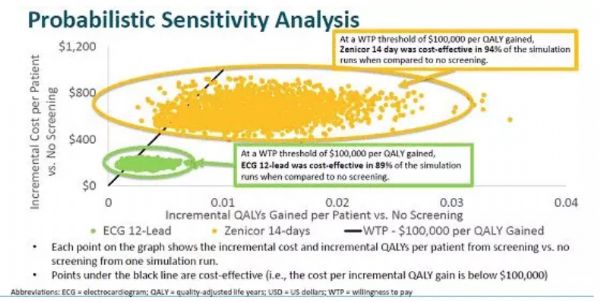
美国当地时间3月11日,在ACC 2018“原创研究亮点:心律失常与临床电生理的年度回顾”专题中,Soeren Mattke教授发布了美国心房颤动筛查费-效比研究的结果。本文特邀复旦大学附属华山医院高秀芳副主任医师点评该研究。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了分享一下
62
学习了分享一下
54
学习了分享一下
61
#ACC#
36
#心房#
28
学习了
68
学习了受益匪浅
57
学习了.涨知识
33
学习了.谢谢分享
19
了解了解.继续关注
29